He has no other significant medical history.
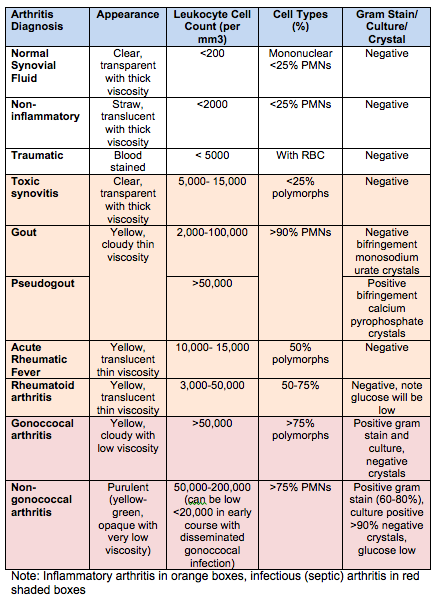
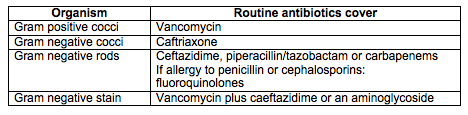
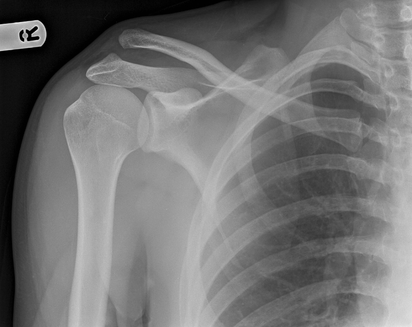
Xrays in ED showed the following:
AP view, lateral split depression fracture - Schatzker type 2
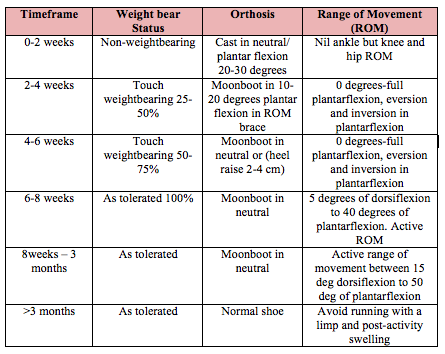
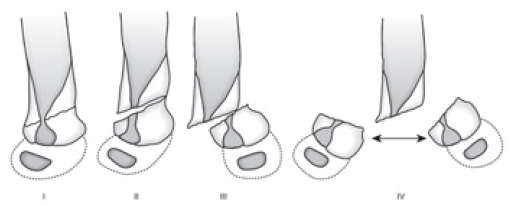
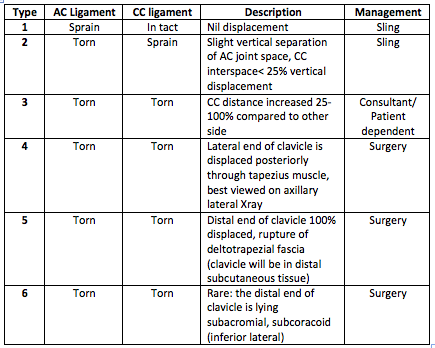
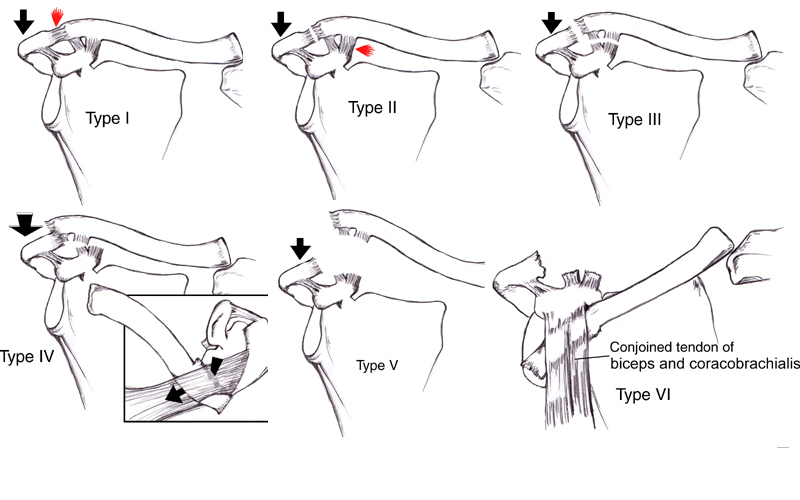
Describe the tibial plateau classifications?
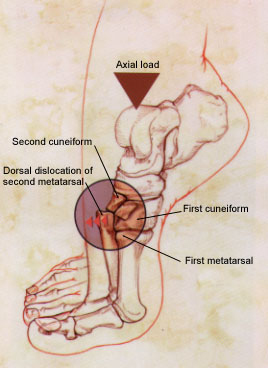
Schatzker Classification is the most commonly used
Type 1: Lateral Split - often young patient, associated with MCL injury, and lateral meniscal entrapment
Type 2: Lateral Split, Depression
Type 3: Pure Lateral Depression - often seen in the elderly
Type 4: Medial Plateau
Type 5: Bicondylar
Type 6: Metaphyseal, Diaphyseal
note: type 4-6 often associated with high velocity trauma
Below images are from orthobullets, Tibial Plateau Fractures (2016)
What factors will immediately change Brad's management?
1. Is the fracture open or closed
2. Is the knee stable - meaning is there more than 10 deg of lateral/medial movement on valgus/varus force. This may be difficult to determine due to patient's pain
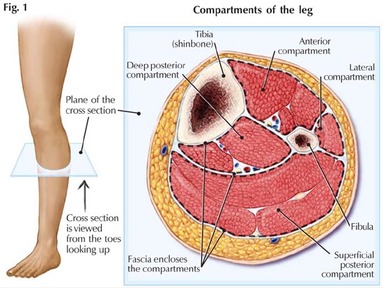
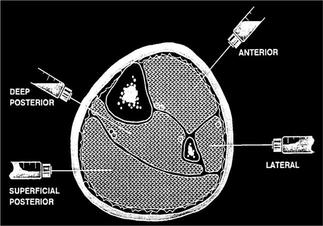
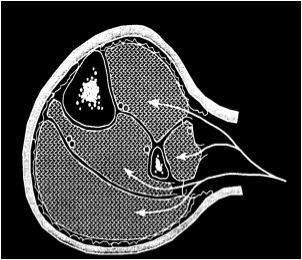
3. Are there signs of compartment syndrome. (See blog below on compartment syndrome)
4. Is Brad neurovascularly intact. Any difference in pulses between Brad's two feet you should also conduct an ankle-brachial index. 'An ABI less than 0.90 has been shown to have a sensitivity exceeding 87% and a specificity exceeding 97% for identifying lower-extremity arterial injury' (Karadsheh, 2016)
Obviously an open fracture, compartment syndrome or poor perfusion requires immediate surgical intervention.
What type of tibial plateau is more likely to be associated with neurovascular injury?
Schatzker type IV are rare and commonly caused by high energy axial load, leading to medial plateau fracture pattern. At the time of the injury their is usually a momentary knee dislocation, where popliteal artery and peroneal nerve are put under tension. Thus it is this type of tibial plateau fracture that is associated with neurovascular compromise due to popliteal artery injury.
What type(s) of tibial plateau injury is more commonly associated with compartment syndrome?
Schatzker type V and VI, is more commonly associated with compartment syndrome and 25% are associated with ACL tears (Karadsheh, 2016).
What type of injury is associated with lateral meniscal injury?
Lateral meniscal injuries are more common than medial in terms of tibial plateau fractures. Schatzker type II injuries are associated with lateral tibial plateau fractures (Karadsheh, 2016).
What investigations would you order?
Xrays:
- AP
- Lateral
- Oblique (good if you suspect depression)
- +/- plateau view (10 deg of caudal tilt)
- important to determine depression and comminution
- ligament and soft tissue injury
Management:
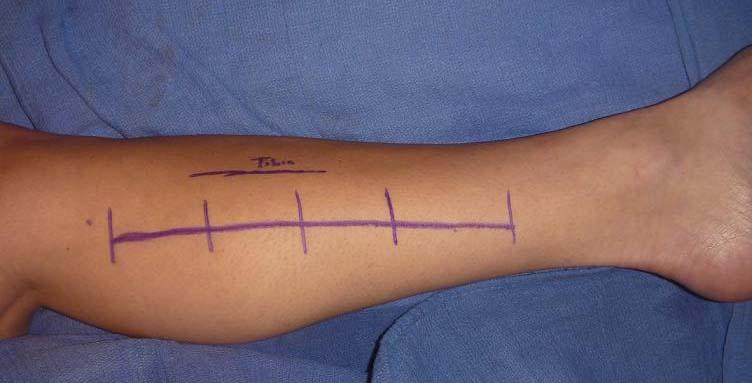
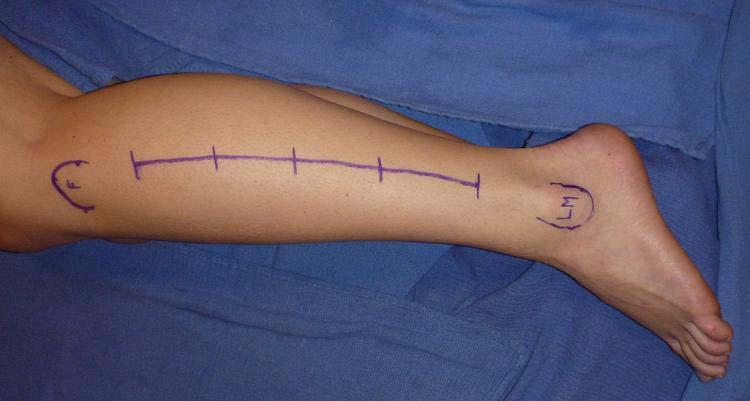
Initial management from ED involves:
- continue non-weightbear patients, analgesia, ice, keep nil by mouth
- calling the orthopaedic registrar on call (additional imaging/operative v non operative management)
- note: tibial plateau fractures (unless neurovascular compromise) will not be operated on for a few days
- normally you will discharge patient home in a Richard's Splint (immobilisation knee brace/backslab) and crutches and referral to orthopaedic outpatient fracture clinic
Indication for Non-Operative Management
1. minimally displaced lateral depression or split fractures
2. minimal trauma injuries with no varus/valgus knee instability
3. non- ambulatory patients
Non operative management involves:
Hinged knee brace, partial weight bear for 8-12 weeks and immediate passive range of movement
Indications for Operative Management (open reduction internal fixation):
1. articular step off greater than 3mm
2. bicondylar fracture
3. medial plateau fracture
4. condylar widening greater than 5mm
5. valgus/varus instability
6. open injury
7. vascular compromise, compartment syndrome
Indications for Operative Management (external fixation):
1. severe open fracture with contamination
2. severe soft tissue injury
Post operative management:
Non or Partial weight bear for 8-12 weeks in hinged knee brace with early ROM
REFERENCES:
Karadsheh, M. (2016). Tibial Palteau Fracture. Orthobullets (3/7/16). Available from: http://www.orthobullets.com/trauma/1044/tibial-plateau-fractures Accessed: 1/4/16.Ip, D. (2006). Tibial Plateau Fractures. In Ip, D (Ed), Orthopedic Traumatology - A Resident's Guide (pp. 421-428). Berlin Heidelberg: Springer.























 RSS Feed
RSS Feed
