Melissa a 26 year old female, RHD, presented to her local GP with ongoing pain and swelling on the ulnar aspect of the base of her right thumb. 2 weeks ago, whilst on a 1 month cycling trip around Europe she fell off her bike and her thumb was forcefully abducted, caught on the bike handle. She had immediate pain but continued her tour. This is the first management she has sought for her thumb.
What is Gamekeepers Thumb?
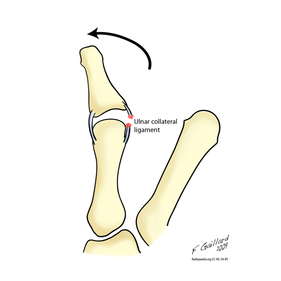
Avulsion or rupture of the ulnar collateral ligament (UCL) - see image below
Mechanism of injury: hyper abduction or extension of MCP joint of thumb
Epidemiology: gamekeepers repetitively stressed the UCL ligament and MCP joint of their thumb when breaking rabbits necks (chronic injury). Today more commonly seen in skiers, also known as 'Skiers Thumb,' occurs when the stock or stock strap forcefully abduct the skiers thumb when falling or aggressively planting the pole (acute injury).
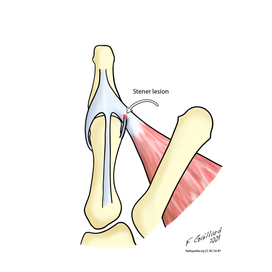
Stener Lesion: UCL ligament avulsed above the adductor aponeurosis. Adductor aponeurosis and adductor pollicis muscle now lying between ligament and proximal phalanx, will not heal without surgical repair.
What is Gamekeepers Thumb?
Avulsion or rupture of the ulnar collateral ligament (UCL) - see image below
Mechanism of injury: hyper abduction or extension of MCP joint of thumb
Epidemiology: gamekeepers repetitively stressed the UCL ligament and MCP joint of their thumb when breaking rabbits necks (chronic injury). Today more commonly seen in skiers, also known as 'Skiers Thumb,' occurs when the stock or stock strap forcefully abduct the skiers thumb when falling or aggressively planting the pole (acute injury).
Stener Lesion: UCL ligament avulsed above the adductor aponeurosis. Adductor aponeurosis and adductor pollicis muscle now lying between ligament and proximal phalanx, will not heal without surgical repair.
Physical Examination specific to UCL ligament rupture:
Appearance and palpation - mass from the torn UCL ligament or bony avulsion may be present on the ulnar aspect of the 1st MCP
Stress MCP joint radially:
Appearance and palpation - mass from the torn UCL ligament or bony avulsion may be present on the ulnar aspect of the 1st MCP
Stress MCP joint radially:
- Neutral position: if lax indicative of accessory UCL injury
- 30 degrees of flexion: if lax indicative of proper UCL injury
- ALWAYS COMPARE TO OTHER SIDE

What imaging would you order?
1. X-rays: AP, lateral, oblique - can show bony avulsion
If there is no bony avulsion, look for ulnar side of the MCP joint, if it appears widened this is suggestive of UCL injury. Stress views were previously undertaken in this situation, however, now there is believed risk of worsening the injury and creating a Stener lesion.
2. Ultrasound scan: to identify tear and Stener lesion, however, operator dependent.
3. MRI: gold standard in identifying; discontinuity of ligament and or joint capsule, boney oedema and Stener lesion.
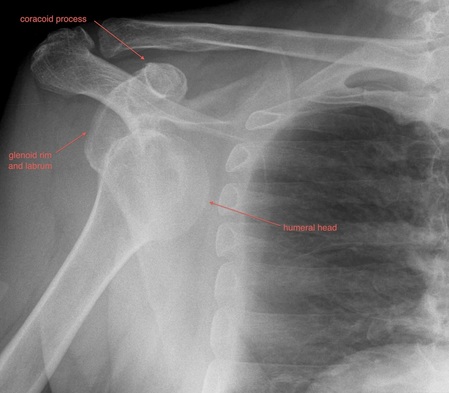
Describe Mel's AP X-ray (image to left):
Always ensure you identify patient and search for old X-rays for comparison, and all views available
There is a minimally displaced intra-articular avulsion fracture of the ulnar aspect of the proximal phalanx of the right thumb.
Always ensure you look for additional fractures, soft tissue swellings, etc. Remember here could be more than one injury.
Treatment Options: Non Operative vs Operative
Non-operative: Immobilise in cast for 4-6 weeks
Indication: partial tears (<20 degrees of side to side variation). (McKean, J. 2014)
Operative:
1. Ligament Repair: using sutures, anchors, screws
2. Ligament Reconstruction: tendon graft
3. MCP Fusion: for chronic injury and pain, often if the above methods have failed
Indication:
References:
Dawes, L., Weerakkody, Y et al. Gamekeepers Thumb. Radiopaedia. Retrieved 27 June 2015 from http://radiopaedia.org/articles/gamekeeper-thumb
Gaillard, F. (2009). Gamekeepers Thumb. Radiopaedia. Retrieved 27 June 2015 from http://radiopaedia.org/articles/gamekeeper-thumb
McKean, J. (2014) Thumb Collateral Ligament Injuries. Orthobullets. Retrieved 27 June 2015 from http://www.orthobullets.com/hand/6040/thumb-collateral-ligament-injury
1. X-rays: AP, lateral, oblique - can show bony avulsion
If there is no bony avulsion, look for ulnar side of the MCP joint, if it appears widened this is suggestive of UCL injury. Stress views were previously undertaken in this situation, however, now there is believed risk of worsening the injury and creating a Stener lesion.
2. Ultrasound scan: to identify tear and Stener lesion, however, operator dependent.
3. MRI: gold standard in identifying; discontinuity of ligament and or joint capsule, boney oedema and Stener lesion.
Describe Mel's AP X-ray (image to left):
Always ensure you identify patient and search for old X-rays for comparison, and all views available
There is a minimally displaced intra-articular avulsion fracture of the ulnar aspect of the proximal phalanx of the right thumb.
Always ensure you look for additional fractures, soft tissue swellings, etc. Remember here could be more than one injury.
Treatment Options: Non Operative vs Operative
Non-operative: Immobilise in cast for 4-6 weeks
Indication: partial tears (<20 degrees of side to side variation). (McKean, J. 2014)
Operative:
1. Ligament Repair: using sutures, anchors, screws
2. Ligament Reconstruction: tendon graft
3. MCP Fusion: for chronic injury and pain, often if the above methods have failed
Indication:
- Acute injury with >20 degrees of varus/valgus instability
- >35 degrees of opening
- Stener lesion: as described and depicted above
References:
Dawes, L., Weerakkody, Y et al. Gamekeepers Thumb. Radiopaedia. Retrieved 27 June 2015 from http://radiopaedia.org/articles/gamekeeper-thumb
Gaillard, F. (2009). Gamekeepers Thumb. Radiopaedia. Retrieved 27 June 2015 from http://radiopaedia.org/articles/gamekeeper-thumb
McKean, J. (2014) Thumb Collateral Ligament Injuries. Orthobullets. Retrieved 27 June 2015 from http://www.orthobullets.com/hand/6040/thumb-collateral-ligament-injury






 RSS Feed
RSS Feed
