Assessment and management of foot injuries and fractures
by Kunal Bhanot
Scenario: called to A&E to assess a 20 year old man who hurt his foot after jumping off a wall. No other injuries.
History
Age
Occupation – useful for deciding treatment
Time/date of injury
Mechanism of injury – direction of torque force to the ankle and the position of the foot - inversion, eversion, impact, fall from height
Immediate problem – pain/swelling, inability to weight bear
Past History
Examination
Attempt to discern fracture versus soft tissue injury.
History
Age
Occupation – useful for deciding treatment
Time/date of injury
Mechanism of injury – direction of torque force to the ankle and the position of the foot - inversion, eversion, impact, fall from height
Immediate problem – pain/swelling, inability to weight bear
Past History
- prior injury to joint causing antecedent laxity and non-acute radiologic
- abnormality.
- chronic medical issues – vasculopathy – may compromise exam results
- use of steroids – considerations for premature osteoporosis
- use of NSAIDs – may mitigate degree of swelling expected
Examination
Attempt to discern fracture versus soft tissue injury.
- Gross deformity, bony tenderness, ecchymosis, discolouration, and inability to weight bear - fracture likely (possibly associated with ligamentous injury)
- Ensure examination of ankle, knee, and proximal fibula - concomitant injuries depending on mechanism
- Plain film imaging generally sufficient
- Apply ankle rules
- Dorsal-plantar, lateral, and oblique views.
- May request weight-bearing views if Lisfranc fracture dislocation is suspected
Management:
Immobilization, ice, and foot elevation with analgesia for all patients with significant foot injuries
Initial immobilization with below knee backslab
Immobilization, ice, and foot elevation with analgesia for all patients with significant foot injuries
Initial immobilization with below knee backslab
Toe Fracture (phalangeal)
Internal metatarsal fracture – 2nd, 3rd, and 4th metatarsals (excluding Lisfranc injury)
- Analgesia
- Generally heal well with minimal therapy
- Buddy tape to adjacent unbroken toe
- Great toe fractures may require reduction and rigid immobilization
- Refer to fracture clinic for follow up
Internal metatarsal fracture – 2nd, 3rd, and 4th metatarsals (excluding Lisfranc injury)
- Analgesia
- Non-displaced and displaced fractures heal well
- Weight-bearing as tolerated
- Cast or rigid-bottom orthopaedic shoe, may use elastic support bandages.
- Fracture clinic <1 week
|
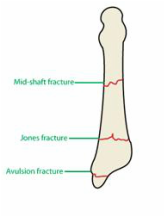
Fifth metatarsal fractures
Lisfranc ligament injury (often associated with avulsion fractures) Causes displacement of 2nd/3rd/4th Metatarsals from the 1st metatarsal. Often subtle and easily missed. Large degree of swelling observed.
|
|
Navicular fracture
Calcaneal fracture Analgesia Often caused by falls from height – high risk for associated injuries – asses ankles, femurs, hips & pelvis and spine Apply backslab, elevation. Investigate with CT scan to determine displacement and articular invovlement. Intra-articular – reduced Böehler’s angle – discuss with senior - possibly for operative fixation. Extra-articular minimally displaced – Immobilization, non-weightbearing. Review fracture clinic 1 week. Extra-articular displaced - may require fixation - discuss with senior. |