Spine
Back pain investigations
A thorough history and clinical examination will provide the clinician with a diagnosis in most cases. History must include specific questions about the ‘red flags’ which, if present, warrant further investigation to ensure there is no serious underlying pathology.
Spine red flags:
Back pain presenting with any of these signs requires urgent investigation with plain Xrays of the spine (which could show evidence of fracture and infection and possibly metastases), bloods (including U&E, CRP, ESR, FBC, Ca2+) and myeloma screen (urine protein electrophoresis looking for Bence-Jones proteins and serum protein electrophoresis). An MRI is a sensitive investigation that can be used to evaluate for important anatomical variations, fractures, tumours, infection and disc pathology that may require urgent treatment.
A thorough history and clinical examination will provide the clinician with a diagnosis in most cases. History must include specific questions about the ‘red flags’ which, if present, warrant further investigation to ensure there is no serious underlying pathology.
Spine red flags:
- New onset of pain age <15 or >50 years of age
- Unexpected weight loss
- Recent illness or systemic infection
- Previous long term steroid use
- Previous history of cancer
- Fever and malaise
- Pain at rest/night pain
- Urinary retention and constipation
- Saddle paraesthesia
Back pain presenting with any of these signs requires urgent investigation with plain Xrays of the spine (which could show evidence of fracture and infection and possibly metastases), bloods (including U&E, CRP, ESR, FBC, Ca2+) and myeloma screen (urine protein electrophoresis looking for Bence-Jones proteins and serum protein electrophoresis). An MRI is a sensitive investigation that can be used to evaluate for important anatomical variations, fractures, tumours, infection and disc pathology that may require urgent treatment.
Lumbar herniation plus radiculopathy (sciatica)
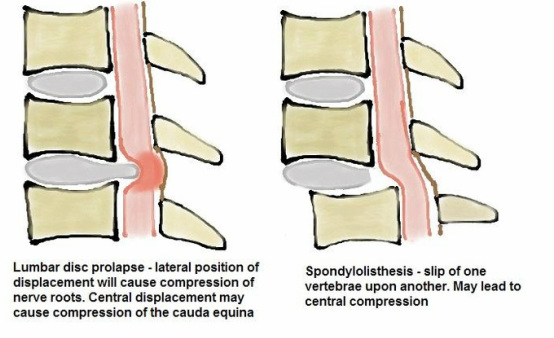
With age, the intervertebral disc becomes dehydrated and the strength and resistance to compressive forces diminishes as the structural proteins and proteoglycans degrade. A tear in the outer fibrous lining of the disc will allow the gelatinous nucleus material to extrude out of the disc. This extruded material or ‘herniation’ may place pressure on the nerve roots crossing the disc, leading to pain radiating to the region supplied by that nerve root.
Most common in the lower lumbar spine due to the highest motion and load-bearing being through these segments, disc herniation is most often at the levels L4-5 and L5-S1. The radiation of pain down the affected limb in the distribution of a specific nerve root is referred to as ‘radicular’. If the pain affects the lower nerve roots, it may be referred to as “sciatica’.
Clinical examination will elicit back pain and probable muscle spasm with limited motion in the lumbar spine combined with pain radiating down the leg to the specific dermatome supplied by the affected nerve root. The pain may be burning or pins and needles and may be accompanied by paraesthesia and weakness in the muscles in that myotome. Nerve root tension signs are elicited by the straight leg raise test (L4-5, L5-S1) or the femoral stretch test (L2-3, L3-4) and indicate that the affected nerve root is tethered by the herniated disc material.
Management
After initial presentation, management with analgesia and a maximum of a week of rest followed by a graduated exercise program under physiotherapy guidance will see 90% of patients recover within 3 months. If there is no improvement, an MRI is required to rule out more sinister causes of pain and to determine the site of herniation. This will allow for treatment with lumbar epidural or X-ray guided nerve-root steroid injections.
With continued symptoms, in carefully selected patients, surgical discectomy has been shown to give a more rapid resolution of symptoms but similar long-term outcomes to nonsurgically treated patients. Surgery does have the rare but potentially fatal complication of injury to the aorta and risk of permanent nerve root injury, so must not be embarked upon lightly.
With age, the intervertebral disc becomes dehydrated and the strength and resistance to compressive forces diminishes as the structural proteins and proteoglycans degrade. A tear in the outer fibrous lining of the disc will allow the gelatinous nucleus material to extrude out of the disc. This extruded material or ‘herniation’ may place pressure on the nerve roots crossing the disc, leading to pain radiating to the region supplied by that nerve root.
Most common in the lower lumbar spine due to the highest motion and load-bearing being through these segments, disc herniation is most often at the levels L4-5 and L5-S1. The radiation of pain down the affected limb in the distribution of a specific nerve root is referred to as ‘radicular’. If the pain affects the lower nerve roots, it may be referred to as “sciatica’.
Clinical examination will elicit back pain and probable muscle spasm with limited motion in the lumbar spine combined with pain radiating down the leg to the specific dermatome supplied by the affected nerve root. The pain may be burning or pins and needles and may be accompanied by paraesthesia and weakness in the muscles in that myotome. Nerve root tension signs are elicited by the straight leg raise test (L4-5, L5-S1) or the femoral stretch test (L2-3, L3-4) and indicate that the affected nerve root is tethered by the herniated disc material.
Management
After initial presentation, management with analgesia and a maximum of a week of rest followed by a graduated exercise program under physiotherapy guidance will see 90% of patients recover within 3 months. If there is no improvement, an MRI is required to rule out more sinister causes of pain and to determine the site of herniation. This will allow for treatment with lumbar epidural or X-ray guided nerve-root steroid injections.
With continued symptoms, in carefully selected patients, surgical discectomy has been shown to give a more rapid resolution of symptoms but similar long-term outcomes to nonsurgically treated patients. Surgery does have the rare but potentially fatal complication of injury to the aorta and risk of permanent nerve root injury, so must not be embarked upon lightly.
Cauda equina syndrome
This is an orthopaedic emergency. A large, central disc herniation at the level of the cauda equina (which are the nerve roots that continue in the spinal canal after the termination of the spinal cord at the level of the L1-2 disc) compressing these nerve roots, patients will usually present with bilateral buttock and lower limb pain (may be pain free) with urinary retention, saddle anaesthesia and possibly constipation. A vital part of the clinical
examination must include digital rectal examination to assess for anal sensation and tone.
The sacral nerve roots are particularly sensitive to ischaemia and delayed decompression of more than 6-12 hours may lead to total loss of function. This can lead to lifelong disability with loss of anal sphincter and bladder control leading to incontinence. Urgent investigation with MRI and surgical decompression give the best prognosis. Delay to diagnosis and treatment is common and leads to a very high number of successful, costly medical negligence claims.
This is an orthopaedic emergency. A large, central disc herniation at the level of the cauda equina (which are the nerve roots that continue in the spinal canal after the termination of the spinal cord at the level of the L1-2 disc) compressing these nerve roots, patients will usually present with bilateral buttock and lower limb pain (may be pain free) with urinary retention, saddle anaesthesia and possibly constipation. A vital part of the clinical
examination must include digital rectal examination to assess for anal sensation and tone.
The sacral nerve roots are particularly sensitive to ischaemia and delayed decompression of more than 6-12 hours may lead to total loss of function. This can lead to lifelong disability with loss of anal sphincter and bladder control leading to incontinence. Urgent investigation with MRI and surgical decompression give the best prognosis. Delay to diagnosis and treatment is common and leads to a very high number of successful, costly medical negligence claims.
Lumbar disc degeneration
Low back pain with limited leg pain is often caused by degeneration of the intervertebral discs with no herniation. Investigated with MRI, an abnormal disc will appear dehydrated and the disc space will be narrowed. Often multiple levels are involved. A discogram may be performed to confirm the causative disc - a high volume of saline is injected into the disc and the levels above and below. Pain upon injection of the suspected disc with an absence of pain upon injection into the other discs confirms the affected level and diagnosis.
Treatment is initiated with analgesia and physical therapy. If a prolonged trial of conservative treatment fails, removal of the pain-causing disc (discectomy), combined with fusion of the vertebrae on either side of it, may be considered.
Low back pain with limited leg pain is often caused by degeneration of the intervertebral discs with no herniation. Investigated with MRI, an abnormal disc will appear dehydrated and the disc space will be narrowed. Often multiple levels are involved. A discogram may be performed to confirm the causative disc - a high volume of saline is injected into the disc and the levels above and below. Pain upon injection of the suspected disc with an absence of pain upon injection into the other discs confirms the affected level and diagnosis.
Treatment is initiated with analgesia and physical therapy. If a prolonged trial of conservative treatment fails, removal of the pain-causing disc (discectomy), combined with fusion of the vertebrae on either side of it, may be considered.
Central canal stenosis
This is narrowing of the spinal canal producing a combination of back and leg pain, due to compression of nerve roots and the thecal sac. It usually occurs in late middle age due to a combination of central disc bulge, hypertrophied facet joints and ligamentum flavum decreasing the central volume of the canal. The canal volume is smallest with the spine extended but flexion increases the available space and patients often find flexing their backs relieves pain.
Symptoms are described as neurogenic claudication with pain worsening with walking but progressing from proximal to distal, pain relieved by sitting or bending and lack of symptoms with cycling (compare with vascular claudication with pain progressing distal to proximal, pain alleviated by stopping activity and pain with cycling).
Investigation is with MRI. Management initiates with analgesia and flexion exercises and may be followed with lumbar epidural steroid injections. Persistent pain impairing the patient’s quality of life may lead to surgery, which involves complete decompression of the spine and may require fusion of the affected levels.
This is narrowing of the spinal canal producing a combination of back and leg pain, due to compression of nerve roots and the thecal sac. It usually occurs in late middle age due to a combination of central disc bulge, hypertrophied facet joints and ligamentum flavum decreasing the central volume of the canal. The canal volume is smallest with the spine extended but flexion increases the available space and patients often find flexing their backs relieves pain.
Symptoms are described as neurogenic claudication with pain worsening with walking but progressing from proximal to distal, pain relieved by sitting or bending and lack of symptoms with cycling (compare with vascular claudication with pain progressing distal to proximal, pain alleviated by stopping activity and pain with cycling).
Investigation is with MRI. Management initiates with analgesia and flexion exercises and may be followed with lumbar epidural steroid injections. Persistent pain impairing the patient’s quality of life may lead to surgery, which involves complete decompression of the spine and may require fusion of the affected levels.
Spondylolisthesis
This is a forward slip of one vertebrae on another. It is caused by pathology at or around the facet joints that stabilise the spine, including abnormal development, stress fracture, degenerative disease and acute fracture. Young patients with mild slips require no treatment but should avoid contact sports. If the slip is more severe, there is a risk of progression and it may cause radicular symptoms or secondary central canal stenosis with
corresponding symptoms. These patients may benefit from surgical fusion in situ. Symptomatic degenerative spondylolisthesis requires surgical decompression and fusion in situ.
This is a forward slip of one vertebrae on another. It is caused by pathology at or around the facet joints that stabilise the spine, including abnormal development, stress fracture, degenerative disease and acute fracture. Young patients with mild slips require no treatment but should avoid contact sports. If the slip is more severe, there is a risk of progression and it may cause radicular symptoms or secondary central canal stenosis with
corresponding symptoms. These patients may benefit from surgical fusion in situ. Symptomatic degenerative spondylolisthesis requires surgical decompression and fusion in situ.
Scoliosis
A curve in the spine, which although a complex 3 dimensional deformity, appears as a lateral deviation with an S- or C-shaped curve. Scoliosis is divided into adult and childhood.
Childhood scoliosis is commonly idiopathic and adolescent but may be related to cerebral palsy and other neuromuscular disorders or congenital spinal abnormalities. The age of presentation, skeletal maturity and rate of progression are the most important factors when deciding upon treatment. Lesser curves and slower progression may be treated conservatively with regular monitoring and intermediate curves with custom-made
thoracolumbosacral braces. The younger the patient is, and the quicker the curve is progressing, the higher the chance of a poor outcome and greater likelihood of requiring surgical correction and fusion.
Adult scoliosis is usually more symptomatic and idiopathic (other causes include degenerate, neuromuscular, post-traumatic and post-surgical). Patients will usually present with pain and a cosmetic deformity. Most are managed non-operatively with analgesia and physical therapy and possibly facet joint injections. Surgery is usually in young, symptomatic adults with progressive, large curves and requires multi-level realignment and fusion.
A curve in the spine, which although a complex 3 dimensional deformity, appears as a lateral deviation with an S- or C-shaped curve. Scoliosis is divided into adult and childhood.
Childhood scoliosis is commonly idiopathic and adolescent but may be related to cerebral palsy and other neuromuscular disorders or congenital spinal abnormalities. The age of presentation, skeletal maturity and rate of progression are the most important factors when deciding upon treatment. Lesser curves and slower progression may be treated conservatively with regular monitoring and intermediate curves with custom-made
thoracolumbosacral braces. The younger the patient is, and the quicker the curve is progressing, the higher the chance of a poor outcome and greater likelihood of requiring surgical correction and fusion.
Adult scoliosis is usually more symptomatic and idiopathic (other causes include degenerate, neuromuscular, post-traumatic and post-surgical). Patients will usually present with pain and a cosmetic deformity. Most are managed non-operatively with analgesia and physical therapy and possibly facet joint injections. Surgery is usually in young, symptomatic adults with progressive, large curves and requires multi-level realignment and fusion.
Infections of the spine
Disc space infections are commonly seen in children, with Staphylococcus aureus being the usual organism. Back pain and tenderness, restricted range of motion and poor walking, sitting or standing represent the clinical picture. Blood tests with raised inflammatory markers and an MRI are diagnostic. Treatment is with appropriate antibiotics.
Vertebral osteomyelitis is becoming more prevalent, typically in elderly, debilitated patients and intravenous drug abusers. Other risk factors include pneumonia, urinary tract infection, diabetes and HIV. The organism is usually seeded via a haematogenous route. Pain, localised tenderness and muscle spasm are usually evident. Plain X-rays may show erosion of vertebral end-plates and disc destruction but MRI and CT-guided aspiration are diagnostic. 6-12 weeks of intravenous antibiotics is the treatment of choice.
Spinal tuberculosis can lead to destruction of several adjacent vertebrae. Abscess formation, neurological compromise due to spinal canal compression (by abscess or bone fragments), meningitis and progressive deformity may occur. Multi-drug therapy is the mainstay of treatment.
Disc space infections are commonly seen in children, with Staphylococcus aureus being the usual organism. Back pain and tenderness, restricted range of motion and poor walking, sitting or standing represent the clinical picture. Blood tests with raised inflammatory markers and an MRI are diagnostic. Treatment is with appropriate antibiotics.
Vertebral osteomyelitis is becoming more prevalent, typically in elderly, debilitated patients and intravenous drug abusers. Other risk factors include pneumonia, urinary tract infection, diabetes and HIV. The organism is usually seeded via a haematogenous route. Pain, localised tenderness and muscle spasm are usually evident. Plain X-rays may show erosion of vertebral end-plates and disc destruction but MRI and CT-guided aspiration are diagnostic. 6-12 weeks of intravenous antibiotics is the treatment of choice.
Spinal tuberculosis can lead to destruction of several adjacent vertebrae. Abscess formation, neurological compromise due to spinal canal compression (by abscess or bone fragments), meningitis and progressive deformity may occur. Multi-drug therapy is the mainstay of treatment.