Assessment and management of pelvic and acetabular trauma
by James Donaldson
Scenario: called to A&E to assess a 34 year old involved in a high speed road traffic accident.
History:
Age – often young, involved in high energy blunt trauma
Assess for other injuries
Time/date of injury
Past medical/surgical history
Last ate / drank – timing of emergency surgery
Medication/drugs and allergies
History:
Age – often young, involved in high energy blunt trauma
Assess for other injuries
Time/date of injury
Past medical/surgical history
Last ate / drank – timing of emergency surgery
Medication/drugs and allergies
Pelvic Trauma
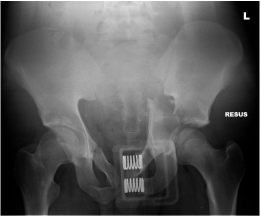
Radiographs / imaging
- Trauma series of x-rays (chest, AP pelvis and lateral cervical spine)
- FAST scan (to rule out intra-abdominal bleeding)
- CT scan only when haemodynamically stable
|
Symptoms and Signs
|
- De-gloving - Flank haematoma
- Do urethrogram prior to Foley. May need supra-pubic catheter - PR and PV mandatory - ?open #
- Anal sphincter tone Inform senior urgently |
|
Advanced Trauma Life Support (ATLS)
|
- Intra-thoracic - Retroperitoneal - Extremity - Pelvic - Venous (80%) - Post venous plexus - Cancellous bone - Arterial (10-20%) - Sup gluteal artery - Int pudendal artery - Obturator artery Trauma team and seniors involved early |
|
External fixator application
Angiography |
|
|
Classification
|
Tile
A) Stable B) Rotationally unstable C) Rotationally and vertically unstable Young and Burgess AP compression type Lateral compression Vertical shear |
BOAST guidelines:
- Early pelvic binder and control of haemorrhage
- PRC, platelets, FFP initially; if ongoing haemorrhage and pelvis is stabilized a laparotomy with pelvic packing +/- embolisation may be needed
- Early CT scan once haemodynamically stable
- High index of suspicion for associated injuries
- Open pelvic fractures may require urgent bladder drainage and bowel diversion by specialists
- Urethral injury diagnosed and managed appropriately
- Definitive plan by pelvic surgeon within 5 days
- Image transfer and referral to specialist centre within 24hrs
- Specialist unit to follow the patient up
Acetabular trauma
|
Symptoms and Signs
|
|
|
Management
|
|
|
Letournel classification
|
|
|
Surgery
|
|
|
Complications
|
|
BOAST guidelines:
- Reduce hip dislocations urgently. Document neurovascular status before and after the procedure. Apply skeletal traction. If irreducible or unstable urgent specialist transfer
- CT scan within 24 hours of hip reduction and early referral / transfer of images
- Reconstruction in a specialist unit within 5 days (no later than 10)
- Chemical thromboprophylaxis within 48hrs of injury assuming no contraindications