Assessment and management of foot injuries and fractures
by Kunal Bhanot
Scenario: called to A&E to assess a 40 year old woman who hurt her ankle after stepping off a curb. No other injuries.
History
Age
Occupation – useful for deciding treatment
Time/date of injury
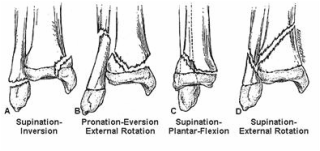
Mechanism of injury – direction of torque force to the ankle and the position of the foot - inversion, eversion, impact, fall from height
Immediate problem – pain/swelling, inability to weight bear
Past History:
Medication/drugs and allergies/time of last meal
History
Age
Occupation – useful for deciding treatment
Time/date of injury
Mechanism of injury – direction of torque force to the ankle and the position of the foot - inversion, eversion, impact, fall from height
Immediate problem – pain/swelling, inability to weight bear
Past History:
- prior injury to joint causing antecedent laxity and non-acute radiologic abnormality.
- chronic medical issues – vasculopathy – may compromise exam results
- use of steroids – considerations for premature osteoporosis
- use of NSAIDs – may mitigate degree of swelling expected
Medication/drugs and allergies/time of last meal
Examination:
Ankle fractures and sprains present with similar symptoms – thorough exam is warranted to prevent unnecessary imaging.
Gross deformity, bony tenderness, ecchymosis, discolouration, and inability to weight bear - suspect fracture. REDUCE any gorss deformity by providing analgesia and providing in-line traction on the limb.
Evidence of vascular compromise requires urgent vascular input.
Ensure examination of ipsilateral knee, proximal fibula, 5th metatarsal
Ankle fractures and sprains present with similar symptoms – thorough exam is warranted to prevent unnecessary imaging.
Gross deformity, bony tenderness, ecchymosis, discolouration, and inability to weight bear - suspect fracture. REDUCE any gorss deformity by providing analgesia and providing in-line traction on the limb.
Evidence of vascular compromise requires urgent vascular input.
Ensure examination of ipsilateral knee, proximal fibula, 5th metatarsal
|
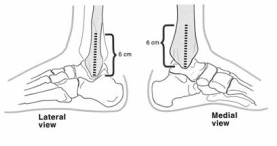
Ottawa Ankle Rules:
Ankle x-ray series required only if bony tenderness in distal 6cm of tibia or fibula, or inability to bear weight both immediately and in the emergency department. Not applicable to patients under 18. Some use absolute threshold of 6 years old and apply rules. Clinical judgement to prevail in patients that are intoxicated, have other distracting injuries, neurovascular compromise, or gross swelling preventing adequate palpation. |
Imaging:
- Apply ankle rules
- Anteroposterior, lateral, and mortise views
- Assess for asymmetrical space around mortise and talar shift.
- May attempt gravity stress views and look for medial widening
- Ring axiom generally holds, eg. Look carefully at medial malleolar architecture of
- lateral malleolus fracture is evident and vice versa.
Stability:
Assess stability of fracture – many classification systems but Denis-Weber is most common:
Assess stability of fracture – many classification systems but Denis-Weber is most common:
- Type A - transverse fibular avulsion fracture, often associated with oblique medial malleolus. Usually stable.
- Type B - oblique fracture of lateral malleolus with or without tibio-fibular syndesmosis rupture and medial injury. May be unstable.
- Type C - high fibular fracture and tibiofibular ligament rupture with medial malleolus transverse avulsion fracture. Usually unstable and require fixation.
Management:
Closed distal ankle fracture - Stable
Ligamentous injury
Closed distal ankle fracture - unstable
Open fracture
Maisonneuve fracture (proximal fibular fracture with disruption of syndesmosis and medial malleolus fracture or disruption of deltoid ligament)
Closed distal ankle fracture - Stable
- Analgesia
- Assess neuro-vascular status
- Apply below knee backslab with stirrup
- Elevate and non-weight bearing
- Monitor for compartment syndrome
- Home with review in fracture clinic <1 week
Ligamentous injury
- Microscopic tear – rest, ice, compression, elevation
- Macroscopic tear – ankle strapped in dorsiflexion 4-6 weeks. Review in fracture clinic 1 week, likely requires physiotherapy.
- Complete tear – below knee walking cast 4-6 weeks. Review in fracture clinic 1 week and physiotherapy.
Closed distal ankle fracture - unstable
- Analgesia
- Assess neuro-vascular status
- Reduce if necessary and apply below knee backslab with stirrup
- Discuss with senior
- Elevate and non-weight bearing
- Monitor for compartment syndrome
- Arrange for operative fixation
Open fracture
- Analgesia
- Assess neuro-vascular status – IF ANY DOUBT, call vascular surgeons
- Call senior urgently
- Remove obvious gross debris
- Place sterile moist gauze on wound
- Apply backslab
- Check tetanus status and administer
- Leave fracture blisters intact
- Antibiotics to be administered
- Book for operative debridement, washout and fixation
Maisonneuve fracture (proximal fibular fracture with disruption of syndesmosis and medial malleolus fracture or disruption of deltoid ligament)
- Examine ankle, particularly for medial tenderness
- Apply backslab
- Discuss with senior - usually require fixation
|
Talus fracture
Analgesia Tenuous blood supply. Risk for AVN If non-displaced fracture – backslab and non-weight-bearing. Fracture clinic <1 week. If displaced fracture or dislocation - urgent senior review. Investigate further with CT scan. May require urgent reduction and fixation Pilon fracture (complex fracture including metaphysis of distal tibial possible talar dome injury)
|
|
Pediatric ankle fractures
|
Distal tibial physial injury:
Generally, undisplaced fractures can be managed non-operatively in below knee backslab and non-weightbearing.
These patients require review in fracture clinic in <1 week.
Any displacement requires further investigation (usually with CT scan) and often require reduction +/- fixation. This should be discussed with a senior.
For comfort, apply backslab and admit for monitoring for compartment syndrome
Generally, undisplaced fractures can be managed non-operatively in below knee backslab and non-weightbearing.
These patients require review in fracture clinic in <1 week.
Any displacement requires further investigation (usually with CT scan) and often require reduction +/- fixation. This should be discussed with a senior.
For comfort, apply backslab and admit for monitoring for compartment syndrome