Assessment and management of acute distal radius fractures
by Zoe Little
Scenario: called to A&E to assess a 64 year old woman who fell on her outstretched hand - no other injuries
History:
Age
Handedness
Occupation
Hobbies/level of function – may be important in deciding definitive treatment plan
Time/date of injury
Mechanism
Altered sensation or motor function distal to the injury
Any other injuries
Past medical/surgical history:
Including previous wrist/forearm problems/surgery
Medication/drugs and allergies
Examination:
Deformity
Ecchymosis
Tenderness
Painful range of motion
Thorough neurovascular assessment, with particular attention to the median nerve
Investigations:
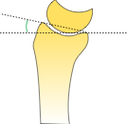
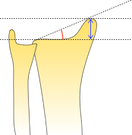
PA and lateral x-rays of the wrist: examine the radiological relationships and consider contralateral views for comparison
History:
Age
Handedness
Occupation
Hobbies/level of function – may be important in deciding definitive treatment plan
Time/date of injury
Mechanism
Altered sensation or motor function distal to the injury
Any other injuries
Past medical/surgical history:
Including previous wrist/forearm problems/surgery
Medication/drugs and allergies
Examination:
Deformity
Ecchymosis
Tenderness
Painful range of motion
Thorough neurovascular assessment, with particular attention to the median nerve
Investigations:
PA and lateral x-rays of the wrist: examine the radiological relationships and consider contralateral views for comparison
Look for associated injuries:
- Widening of the scapholunate interval (suggestive of scapholunate ligament injury)
- Interruption of Gilula’s lines (carpal instability)
- Consider CT to further demonstrate the extent of any intra-articular involvement
Classification
Descriptive:
Open vs closed
Displacement
Angulation
Comminution
Loss of radial length
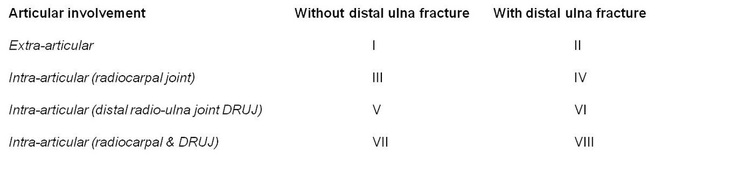
Frykman:
Open vs closed
Displacement
Angulation
Comminution
Loss of radial length
Frykman:
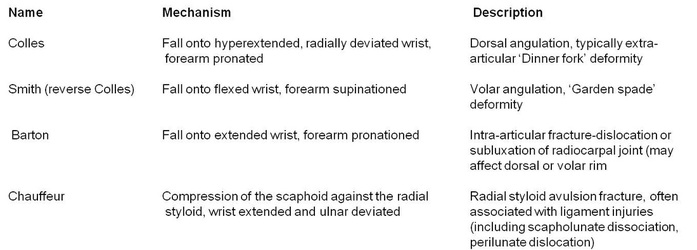
Eponymous fractures
Management
Aim to restore anatomy and regain function - displaced fractures should undergo closed reduction in the emergency department.
Dependent upon fracture pattern and patient factors
Non-operative treatment
Closed reduction (if displaced) and cast immobilisation for 6 weeks
Indications:
Palmar (volar) tilt - up to 5o dorsal angulation
Radial inclination - less than 5o loss
Intra-articular step - less than 2mm
Dependent upon fracture pattern and patient factors
Non-operative treatment
Closed reduction (if displaced) and cast immobilisation for 6 weeks
Indications:
- Undisplaced and minimally displaced fractures
- Displaced fractures which have been reduced to achieve:
Palmar (volar) tilt - up to 5o dorsal angulation
Radial inclination - less than 5o loss
Intra-articular step - less than 2mm
Techniques
Closed reduction (dorsally angulated fracture):
Closed reduction (dorsally angulated fracture):
|
Stages
Perform a haematoma block
|
Equipment required
Gloves Blunt fill or 21G needle to draw up 23G needle to administer block 10ml syringe 1% lidocaine - 2mg/kg (0.2ml/kg) Chlorhexidine spray Adhesive dressing An assistant is required - to apply counter-traction and apply backslab whist traction and reduction are maintained |
Reduction
Hyperextend the distal fragment, then apply traction to reduce the distal fragment onto the proximal fragment
Hyperextend the distal fragment, then apply traction to reduce the distal fragment onto the proximal fragment
Apply backslab
Apply a well moulded backslab with the wrist in slight flexion (<15o)
Check x-ray
Repeat AP and lateral radiographs
Apply a well moulded backslab with the wrist in slight flexion (<15o)
Check x-ray
Repeat AP and lateral radiographs
Operative treatment
Options:
Percutaneous pinning
External fixation
Open reduction and internal fixation (dorsal or volar plating)
Indications:
Options:
Percutaneous pinning
External fixation
Open reduction and internal fixation (dorsal or volar plating)
Indications:
- Radial shortening >5mm
- Dorsal angulation >5o
- Loss of radial inclination >5o
- Displaced intra-articular fracture (step>2mm)
- Volar or dorsal comminution
- Unstable fracture pattern (e.g. Smith’s fracture)
- Loss of reduction following non-operative treatment