Assessment and management of the septic native joint
by James Donaldson
Scenario: called to A&E to assess a patient with a painful hip with no precipitating events
History:
Age – often paediatric, immunosuppressed or elderly.
Time/date of onset. Systemic symptoms.
Paediatric history and risk factors for infection
Prodromal symptoms
Past medical/surgical history
Medication/drugs and allergies
Last ate/drank (for timing of emergency surgery if needed)
History:
Age – often paediatric, immunosuppressed or elderly.
Time/date of onset. Systemic symptoms.
Paediatric history and risk factors for infection
Prodromal symptoms
Past medical/surgical history
Medication/drugs and allergies
Last ate/drank (for timing of emergency surgery if needed)
|
Aetiology:
Pre-disposing factors:
Clinical features:
|
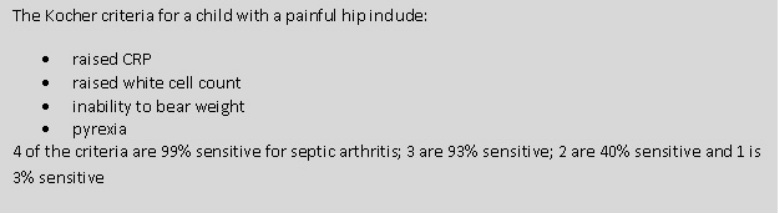
Investigations:
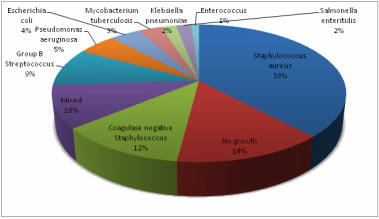
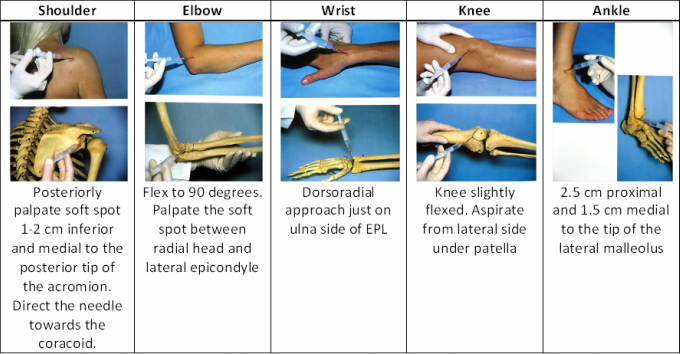
Joint aspiration with microscopy and culture of joint fluid is diagnostic. Ultrasound is useful and an aspiration can be performed at the same time, especially for deeper joints like the hip.
Aspiration MUST be done under sterile conditions to ensure infection is not introduced.
- Raised white cell count, CRP and ESR
- Blood cultures may be positive
- X-rays may help to exclude other causes of painful joint
Joint aspiration with microscopy and culture of joint fluid is diagnostic. Ultrasound is useful and an aspiration can be performed at the same time, especially for deeper joints like the hip.
Aspiration MUST be done under sterile conditions to ensure infection is not introduced.
- Synovial fluid examination is the gold standard
- A white cell count greater than 50,000 per ml is usually suggestive of infection
Differential diagnosis:
- Acute osteomyelitis. The two may co-exist in young children - the treatment is the same.
-
Trauma: synovitis or
haemarthrosis (x-ray may show intra-articular fracture)
-
Irritable joint (the
child will be systemically well) with normal blood tests
-
Crystal monoarthropathy (gout or pseudogout)
- Haemophiliac bleed
Management:
If blood tests, examination and clinical picture support septic arthritis, it is an EMERGENCY. Senior doctors must be informed and the patient prepared for urgent joint washout. Delay to surgery will lead to greater destruction of joint cartilage.
Antibiotics: initially best guess broad-spectrum intravenous antibiotics (changed when sensitivities are known)
Intravenous antibiotics may be converted to oral antibiotics once signs of sepsis have resolved and then continued for 6 weeks.
If blood tests, examination and clinical picture support septic arthritis, it is an EMERGENCY. Senior doctors must be informed and the patient prepared for urgent joint washout. Delay to surgery will lead to greater destruction of joint cartilage.
- Supportive treatment with IV fluids, analgesia and splintage
-
URGENT surgical
drainage and washout.
- A further washout may be needed if symptoms do not settle within 24-48 hours.
Antibiotics: initially best guess broad-spectrum intravenous antibiotics (changed when sensitivities are known)
Intravenous antibiotics may be converted to oral antibiotics once signs of sepsis have resolved and then continued for 6 weeks.
Prognosis:
Predictors of poor outcome include:
- 30% of adults with septic arthritis are left with reduced ROM or chronic pain after infection
- Bone destruction and dislocation (especially the hip) may occur
- Cartilage destruction may lead to ankylosis or secondary osteoarthritis
- Growth disturbance and deformity occur in children
Predictors of poor outcome include:
- Age >60y
- Infection of hip or shoulder joint
- Underlying rheumatoid arthritis
- Positive findings on synovial fluid cultures 7 days after starting antibiotics
- Delay in treatment