You are an orthopaedic registrar and an ED intern calls you with the following case:
60 y.o M, Jo, BMI 35, presented to ED with a 2 day history of Atraumatic pain in his right hip, subjective rigors, inability to weight bear over the last day. He previously had a right total hip replacement 10 years ago, with no complaints since. He denies any other focal infective symptoms (ie no cough, dysuria, wounds, etc)
What risk factors are associated with septic arthritis, or what other questions would you ask the patient?
Risk factors for septic arthritis can be broke up into how the organism would have spread to the infected joint, (that is how I like to break it up in my mind). You would ask Jo the following:
Contiguous Spread:
· Skin infection – Jo denies
Direct inoculation:
· Previous intra-articular injection
· Prosthetic joint – which you know he has, look at timing, operative notes, infection at the time – 10 years ago, nil complication
· Recent joint surgery – denies
Haematogenous Spread/Immunocompramised
· Diabetes – yes T2DM, managed with oral medication only
· Immunocompromised – Jo denies any Hx of auto-immune diseases, HIV, imunosuprpressive medication
· IV drug user – denies
· Other causes of sepsis – septic screen done by ED has been negative
Other questions:
· Injury to hip/ trauma - denies
· Hx of gout - denies
· Osteoarthritis- yes
Risk factors for the development of prosthetic joint infections include previous fracture, seropositive rheumatoid arthritis, high body mass index, revision arthroplasty, and surgical site infections. Jo's only risk factor is his high body mass index. Septic arthritis in prosthetic joints after 24 months are normally caused by haematogenous spread (Barilla-LaBarca, M. Horowitz, D. Horowitz, S. 2011)
60 y.o M, Jo, BMI 35, presented to ED with a 2 day history of Atraumatic pain in his right hip, subjective rigors, inability to weight bear over the last day. He previously had a right total hip replacement 10 years ago, with no complaints since. He denies any other focal infective symptoms (ie no cough, dysuria, wounds, etc)
What risk factors are associated with septic arthritis, or what other questions would you ask the patient?
Risk factors for septic arthritis can be broke up into how the organism would have spread to the infected joint, (that is how I like to break it up in my mind). You would ask Jo the following:
Contiguous Spread:
· Skin infection – Jo denies
Direct inoculation:
· Previous intra-articular injection
· Prosthetic joint – which you know he has, look at timing, operative notes, infection at the time – 10 years ago, nil complication
· Recent joint surgery – denies
Haematogenous Spread/Immunocompramised
· Diabetes – yes T2DM, managed with oral medication only
· Immunocompromised – Jo denies any Hx of auto-immune diseases, HIV, imunosuprpressive medication
· IV drug user – denies
· Other causes of sepsis – septic screen done by ED has been negative
Other questions:
· Injury to hip/ trauma - denies
· Hx of gout - denies
· Osteoarthritis- yes
Risk factors for the development of prosthetic joint infections include previous fracture, seropositive rheumatoid arthritis, high body mass index, revision arthroplasty, and surgical site infections. Jo's only risk factor is his high body mass index. Septic arthritis in prosthetic joints after 24 months are normally caused by haematogenous spread (Barilla-LaBarca, M. Horowitz, D. Horowitz, S. 2011)
What investigations would you have expected the intern to have ordered?
1. Bloods, which revealed:
WCC 11.4
CRP 40
ESR 10 (note ESR is often normal in early infection, rises after 2 days, returns to normal after 3-4 weeks)
Remainder of bloods - NAD
2. Full septic screen
Blood cultures – pending
CXRAY
Urine
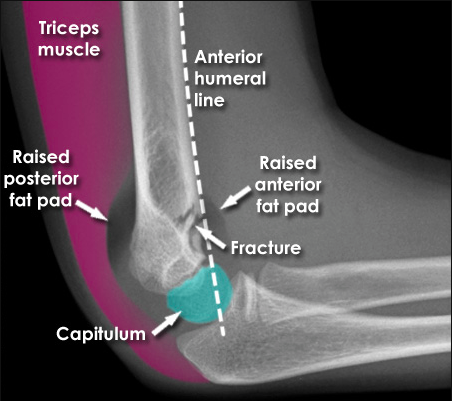
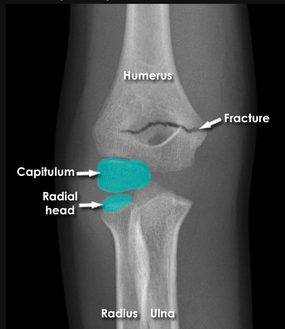
3. Imaging: Hip Xray – AP and lateral view: this is to determine if there is any obvious joint effusion, peri-prosthetic fracture, dislocation, etc.
You called the radiology registrar on call, to discuss additional imaging as you knew a CT would have significant artifact due to the patient’s right total hip replacement.
He consequently had an ultrasound guided joint aspirate of his right hip. The synovial fluid aspirated was purulent in appearance, indicative of an infective arthritis.
NOTE: Commonly doctors will disregard a CRP of 40 and WCC 11.4, as it is not indicative of septic arthritis, orthopaedic registrars would expect a CRP much higher. However, it is important to assess the patient clinically and if uncertain an aspirate is definitive. It is also important to remember that patients with a prosthetic joint that intraarticular WCC cutoffs may be as low as 1,1000 per mm3, making diagnosis problematic (Barilla-LaBarcam M 2001)
Jo's repeat CRP the next day was 289...
Hip aspirate was taken under ultrasound guidance. What would you put on the pathology form?
(PCR testing may help isolate less common organisms, such as Borelia species and if gonococcal infection suspected).
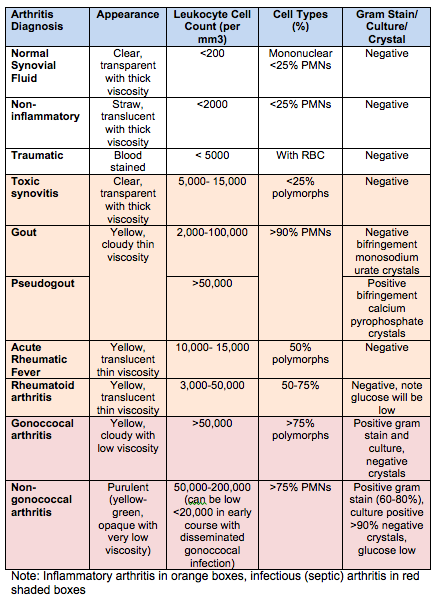
Interpret the following results:
WCC: 75,000
PMN (polymorphnuclear) 90%
Crystals: negative
Gram stain: Gram-positive cocci
Culture: positive
- Gram stain
- Cell count with differential
- Crystal analysis
- Microscopy, culture and sensitivities
- Glucose analysis: in bacterial infection or tuberculosis, the synovial fluid glucose will be less than half the serum value. Occasionally, low values may be seen in RA.
(PCR testing may help isolate less common organisms, such as Borelia species and if gonococcal infection suspected).
Interpret the following results:
WCC: 75,000
PMN (polymorphnuclear) 90%
Crystals: negative
Gram stain: Gram-positive cocci
Culture: positive
Remember.. even if crystals are positive, a patient can have a crystal arthropathy and septic arthritis at one time.
What are the most common microorganism causing septic arthritis?
Majority 80% of septic arthritis is caused by nongonococcal pathogens (most commonly Staphylococcus species (Barilla-LaBarcam M, et al 2010).
Non-Gonoccocal
Gram-positive staphylococci
Gonoccocal:
Gram negative cocci: neisseria gonorrhea
Others:
Management:
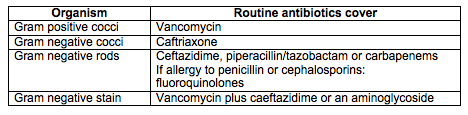
Gram stain results should direct initial antibiotic treatment: See table below for appropriate cover.
What are the most common microorganism causing septic arthritis?
Majority 80% of septic arthritis is caused by nongonococcal pathogens (most commonly Staphylococcus species (Barilla-LaBarcam M, et al 2010).
Non-Gonoccocal
Gram-positive staphylococci
- Associated with: drug abuse, cellulitis, abscesses, endocarditis, and chronic osteomyelitis
- Staphylococcus aureus: most common in developed countries
- Methicillin-resistant S. aureus (MRSA): 5-25%, associated with older population, often involves the shoulder joint and health care (nursing home) patients
- Streptococcus species: second most common
- Associated with: urinary tract infections, intravenous drug use, older age, compromised immune system, and skin infections.
- Pseudomonas aeruginosa and Escherichia coli (most common)
Gonoccocal:
Gram negative cocci: neisseria gonorrhea
- most common organism in otherwise healthy sexually active adolescents and young adults
- knee most commonly involved
- cultures should be taken from mucosal sites (e.g., urethra, rectum, pharynx, cervix)
Others:
- salmonella: associated with sickle cell disease
- pseudomonas aeruginosa: associated with history of IV drug abuse
- pasteurella multocida: associated with dog or cat bite
- eikenella corrodens: associated with human bite
- organism found in immunocompromised host can include fungal, and candida common pathogens
Management:
Gram stain results should direct initial antibiotic treatment: See table below for appropriate cover.
How was Jo's septic arthritic hip managed?
Jo was managed by an urgent washout and tissue sample in theatre. He will most likely require a repeat washout and removal/replacement of metalwork.
Emperic intravenous antibiotics were commenced once gram stain was available. Microbiology and infectious disease was contacted to determine ideal antibiotic therapy and duration for Jo. Jo was initially managed with vancomycin. He required 4 weeks of intravenous cover and then was changed to oral antibiotics, based on microbiology and clinical response.
REFERENCES:
Abassi, D. (2015). Septic Arthritis - Adult. Orthobullets. Accessed 7/8/15. Available from: http://www.orthobullets.com/trauma/1058/septic-arthritis--adult.
Mandell, G. Bennett, J. Dolin, R. (2010). Infectious arthritis of native joints. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa.: Churchill Livingstone; 2010:1443–1456.
Ghanem E, Parvizi J, Burnett RS, et al. Cell count and differential of aspirated fluid in the diagnosis of infection at the site of total knee arthroplasty. J Bone Joint Surg Am. 2008;90(8):1637–1643.
Barilla-LaBarca, M. Horowitz, D. Horowitz, S. (2011) Approach to Septic Arthritis. Am Fam Physician. 2011 Sep 15;84(6):653-660. Accessed 8/8/15. Available from: http://www.aafp.org/afp/2011/0915/p653.html
Jo was managed by an urgent washout and tissue sample in theatre. He will most likely require a repeat washout and removal/replacement of metalwork.
Emperic intravenous antibiotics were commenced once gram stain was available. Microbiology and infectious disease was contacted to determine ideal antibiotic therapy and duration for Jo. Jo was initially managed with vancomycin. He required 4 weeks of intravenous cover and then was changed to oral antibiotics, based on microbiology and clinical response.
REFERENCES:
Abassi, D. (2015). Septic Arthritis - Adult. Orthobullets. Accessed 7/8/15. Available from: http://www.orthobullets.com/trauma/1058/septic-arthritis--adult.
Mandell, G. Bennett, J. Dolin, R. (2010). Infectious arthritis of native joints. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa.: Churchill Livingstone; 2010:1443–1456.
Ghanem E, Parvizi J, Burnett RS, et al. Cell count and differential of aspirated fluid in the diagnosis of infection at the site of total knee arthroplasty. J Bone Joint Surg Am. 2008;90(8):1637–1643.
Barilla-LaBarca, M. Horowitz, D. Horowitz, S. (2011) Approach to Septic Arthritis. Am Fam Physician. 2011 Sep 15;84(6):653-660. Accessed 8/8/15. Available from: http://www.aafp.org/afp/2011/0915/p653.html










 RSS Feed
RSS Feed
