
Dan, an orthopaedic consultant, and avid wrestler presented to the ED department with right sided shoulder pain and deformity post falling onto his right shoulder during a wrestling match. He suspects he has an AC joint disruption and as you are a junior doctor in ED he starts questioning your knowledge.
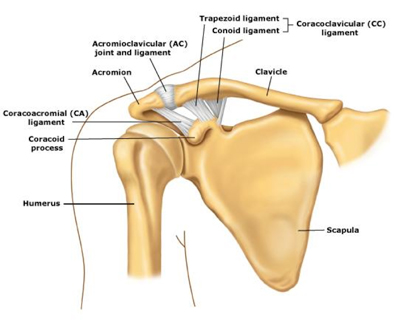
"What ligaments stabilise AC joint?"
As you have read junior bones you keenly answer, "the ACJ stabalised by the..:
1. Acromioclavicular ligament: provides horizontal stability, has 4 components (superior, inferior, anterior and posterior component)
2. Coricoclavicular ligaments: provides vertical stability, this is comprised of:
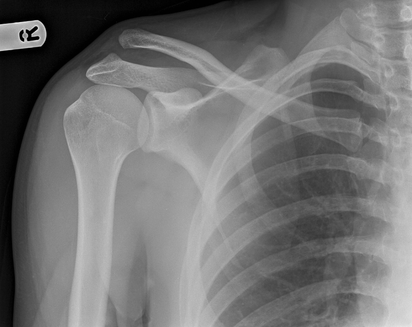
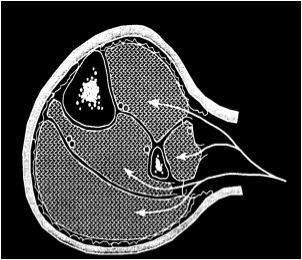
Dr Dan's Xray is below, please interpret..
1. Acromioclavicular ligament: provides horizontal stability, has 4 components (superior, inferior, anterior and posterior component)
2. Coricoclavicular ligaments: provides vertical stability, this is comprised of:
- Trapezoid ligament: located 3 cm from the lateral end of the clavicle
- Conoid ligament: located 4.5cm from the lateral end of the clavicle
Dr Dan's Xray is below, please interpret..
Remember to go back to basic principles: identify patient, date, view and see if there are previous Xrays and additional views. Also ensure you have imaging of the contralateral ACJ for comparison.
The above AP Xray demonstrates widening of the right coricoclavicular distance, the right clavicle is superiorly displaced 100% (normally compared to other side), suggestive of a type 3 acromioclavicular distance, however, additional views would be required to confirm this.
Note: to visualize the AC ligament you can ask for imaging at 1/3 penetration
What other imaging (views) would you order?
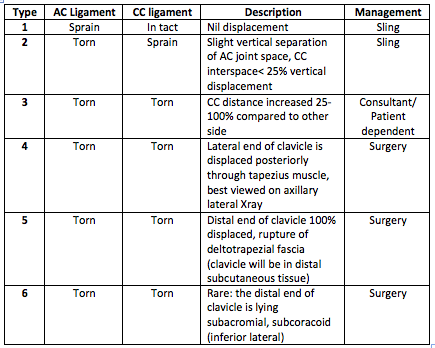
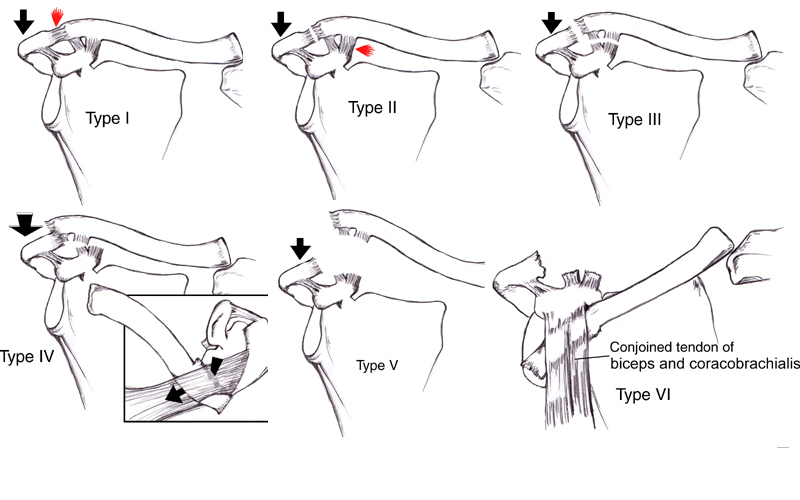
Describe Rockwell Classification of AC Joint Injuries:
The above AP Xray demonstrates widening of the right coricoclavicular distance, the right clavicle is superiorly displaced 100% (normally compared to other side), suggestive of a type 3 acromioclavicular distance, however, additional views would be required to confirm this.
Note: to visualize the AC ligament you can ask for imaging at 1/3 penetration
What other imaging (views) would you order?
- Axillary lateral: required to diagnose type 4
- Zanca view: tilt the Xray 10-15deg towards cephalic direction and using only 50% of the standard AP penetration strength
Describe Rockwell Classification of AC Joint Injuries:
What are the management options for Dr Dan's Grade 3 ACJ injury?
Remember: conservative vs operative
And the 4 basic principles: reduce, fix, wait, rehabilitate
Conservative Management
Indication: Types 1, 2, 3 (not in labourers, elite athletes)
ICE, rest and sling for 3 weeks
Rehabilitation: early ROM, regain functional movement by 6 weeks and return to normal activity by 12 weeks
Complications : ACJ arthritis, chronic subluxation and instability
vs
Operative Management: ORIF or ligament reconstruction
Indication: Types 3 (labourers, athletes), 4, 5, 6
Contraindications: poor compliance with post operative rehabilitation, skin problems over surgical site
Rehabilitation: sling, with no abduction for 6 weeks, no shoulder ROM for 6 weeks, return to normal activity at 6 months
ORIF with hook plate:
ORIF with CC suture fixation:
ORIF with screw fixation:
CC Ligament reconstruction: with free tendon graft OR Modified Weaver-Dunn (transfer of coracoacromial ligament to the distal clavicle to recreate CC ligament)
Remember: conservative vs operative
And the 4 basic principles: reduce, fix, wait, rehabilitate
Conservative Management
Indication: Types 1, 2, 3 (not in labourers, elite athletes)
ICE, rest and sling for 3 weeks
Rehabilitation: early ROM, regain functional movement by 6 weeks and return to normal activity by 12 weeks
Complications : ACJ arthritis, chronic subluxation and instability
vs
Operative Management: ORIF or ligament reconstruction
Indication: Types 3 (labourers, athletes), 4, 5, 6
Contraindications: poor compliance with post operative rehabilitation, skin problems over surgical site
Rehabilitation: sling, with no abduction for 6 weeks, no shoulder ROM for 6 weeks, return to normal activity at 6 months
ORIF with hook plate:
- Approach: exposure of middle and distal clavicle, hook plate positioned over superior distal clavicle and ‘hooked’ under the acromian.
- Pros and cons: rigid fixation, often requires removal of plate, high rate of acromial wea.
ORIF with CC suture fixation:
- Approach: proximal aspect of anterolateral approach to the shoulder
- Technique: suture placed around/through clavicle and around the base of the coracoid (+/- suture anchors for coracoid fixation)
- Pros and cons: requires careful suture passage inferior to coracoid. Minimal risk of hardware failure or migration, suture not as strong as screw fixation.
ORIF with screw fixation:
- Approach: proximal aspect of the anteriorlateral approach to the shoulder
- Technique: screw from distal clavicle into coracoid
- Pros and cons: rigid fixation, danger of screw damaging critical structure below coracoid, complicated by hardware irritation or failure.
CC Ligament reconstruction: with free tendon graft OR Modified Weaver-Dunn (transfer of coracoacromial ligament to the distal clavicle to recreate CC ligament)
- Approach: proximal aspect of the anteriorlateral approach to the shoulder +/- harvest site (hamstring/Palmaris tendon)
- Pros and cons: coracoacromial ligament not as strong as normal CC ligament vs graft which recreates strength of native CC ligament but standard risk of graft use.
Above is Dr Dan's post operative Xray. He was managed with corico-clavicular suture fixation.
REFERENCES:
Abbasi, D. Badylak, J. 2015. Acromio-Clavicular Injuries (AC Seperation). Orthobullets. Accessed: 15/7/15
Caribbean Sports Orthopaedic Clinic, 2010. ACJ Reconstruction. Available from: https://www.c-soc.com/surgical/treatments/shoulder/acj-reconstruction/ Accessed: 20/7/15
Sinnerton, R. ACJ (Hook Plate, Surgilig) Available from: http://www.lu-lu.co.uk/operations/acromio-clavicular-joint/ Accessed: 17/7/15.
The Physio Lounge, 2014. Skiing Injuries. Available at http://www.physiolounge.co.uk/skiing-injuries/. Accessed: 14/7/15
REFERENCES:
Abbasi, D. Badylak, J. 2015. Acromio-Clavicular Injuries (AC Seperation). Orthobullets. Accessed: 15/7/15
Caribbean Sports Orthopaedic Clinic, 2010. ACJ Reconstruction. Available from: https://www.c-soc.com/surgical/treatments/shoulder/acj-reconstruction/ Accessed: 20/7/15
Sinnerton, R. ACJ (Hook Plate, Surgilig) Available from: http://www.lu-lu.co.uk/operations/acromio-clavicular-joint/ Accessed: 17/7/15.
The Physio Lounge, 2014. Skiing Injuries. Available at http://www.physiolounge.co.uk/skiing-injuries/. Accessed: 14/7/15



 RSS Feed
RSS Feed
