You are on night ward call and a nurse calls you to review a post operative patient for worsening leg pain. James, a 25 year old male, is day 1 post right intramedullary tibial nail. You have been called multiple times about James for pain relief. He has low pain tolerance and is suspected to use regular recreational drugs.
What questions would you ask the nurse?
REMEMBER: compartment syndrome can occur wherever skeletal muscle is surrounded by fascia, including leg (similar to this case), forearm, hand, foot, thigh, buttocks, shoulder, etc
Pathophysiology of compartment syndrome
What are the 6 P's of Compartment Syndrome and what are late and early signs? Hint: think of the pathophysiology above (Stracciolini, Hammerberg 2015)
Interpreting Clinical Findings:
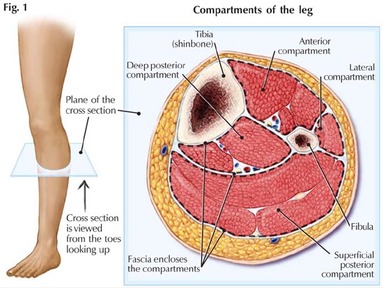
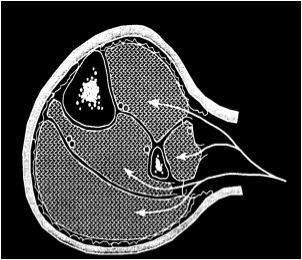
What are the 4 compartments of the leg and define what structures are within them?
1. Anterior Compartment:
2. Lateral Compartment
3. Deep Posterior Compartment
4. Superfical Posterior Compartment
REMEMBER: you will never get told off for removing a cast if you suspect compartment syndrome
How to measure compartment pressures?
What questions would you ask the nurse?
- Neurovascular observations - including capillary refill
- Amount of analgesia used
- Background
- known bleeding disorder
- does he have a cast in situ
REMEMBER: compartment syndrome can occur wherever skeletal muscle is surrounded by fascia, including leg (similar to this case), forearm, hand, foot, thigh, buttocks, shoulder, etc
Pathophysiology of compartment syndrome
- trauma/ soft tissue destruction
- bleeding and oedema
- increased interstitial pressure
- vascular occlusion
- myoneural compromise
What are the 6 P's of Compartment Syndrome and what are late and early signs? Hint: think of the pathophysiology above (Stracciolini, Hammerberg 2015)
- Pain on passive stress - early sign - most sensitive
- Palpable swelling - woodlike
- Paraesthesia -reduced sensation secondary to ischaemic nerve dysfunction
- Poikilothermia
- Pallor - unusual finding
- Peripheral pulses absent - late finding
Interpreting Clinical Findings:
- Capillary refill becomes compromised if compartment pressure reaches 25-30mmHg of mean arterial pressure
- Pain develops with compartment pressure of 20-30mmHg
- Ischaemia occurs if compartment pressure reaches diastolic pressure
What are the 4 compartments of the leg and define what structures are within them?
1. Anterior Compartment:
- Function: dorsifllexion of foot and ankle
- Muscles within compartment: tibialis anterior, extensor hallucis longus, extensor digitorum longus, peroneus tertius
2. Lateral Compartment
- Function: plantarflexion and eversion of foot
- Muscles within compartment: peroneus (fibularis) longus, peroneus brevis
- Nerve: isolated lateral compartment syndrome would affect superficial peroneal nerve
3. Deep Posterior Compartment
- Function: plantarflexion and inversion of foot
- Muscles: tibialis posterior, felxor digitorum longus, flexor hallucis longus
4. Superfical Posterior Compartment
- Function: plantarflexion of foot and ankle
- Muscles: gastrocnemius, soleus, plantaris
REMEMBER: you will never get told off for removing a cast if you suspect compartment syndrome
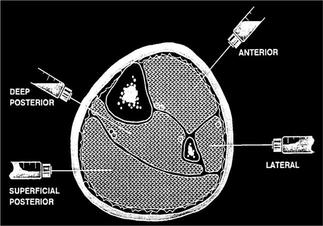
How to measure compartment pressures?
How do I measure compartments?
3 methods are used frequently:
1. A handheld manometer (eg, Stryker device)
2. A simple needle manometer system, and
3. The wick or slit catheter technique
Both manometer methods involve injecting a small quantity of saline into a closed compartment and measuring the resistance from tissue pressure
The normal pressure of a tissue compartment falls between 0 and 8 mmHg (Klenerman L, 2007)
Procedure:
Should aim to measure pressures within 5cm of fracture site.
3 methods are used frequently:
1. A handheld manometer (eg, Stryker device)
2. A simple needle manometer system, and
3. The wick or slit catheter technique
Both manometer methods involve injecting a small quantity of saline into a closed compartment and measuring the resistance from tissue pressure
The normal pressure of a tissue compartment falls between 0 and 8 mmHg (Klenerman L, 2007)
Procedure:
Should aim to measure pressures within 5cm of fracture site.
- Anterior Compartment: enter perpendicular to skin 1cm lateral to anterior border of tibia
- Deep Posterior Compartment: enter perpendicular to skin, just posterior to the medial border of tibia
- Superficial Posterior Compartment: enter middle of calf
- Lateral Compartment: enter just anterior to posterior border of fibula
Treatment:
Non-operative:
1. Bi-Valve James' cast
2. Observe: if not consistent with compartment syndrome
3. Hyperbaric oxygen therapy: increases oxygen diffusion gradient
Operative: Emergent fasciotomy of all four compartments
Indications:
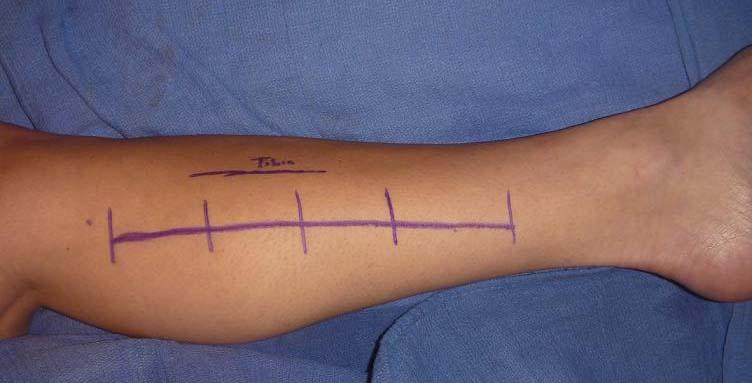
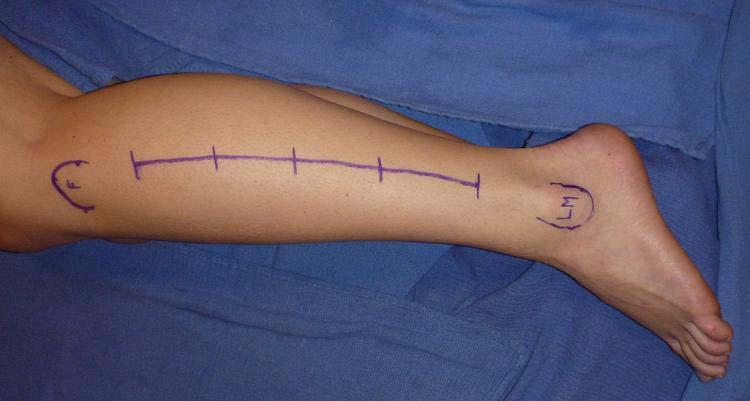
1. Dual (2 incisions) medial and lateral incision: 2 x 15 cm incisions
Non-operative:
1. Bi-Valve James' cast
2. Observe: if not consistent with compartment syndrome
3. Hyperbaric oxygen therapy: increases oxygen diffusion gradient
Operative: Emergent fasciotomy of all four compartments
Indications:
- Compartment pressures of 30-45mmHg
- Clinical presentation with compartment syndrome
- Compartment pressures within 30mmHg of diastolic BP
1. Dual (2 incisions) medial and lateral incision: 2 x 15 cm incisions
2. Single lateral incision from head of fibula to ankle along line of fibula
REFERENCES
Karadsheh, M. 2015 Leg Compartment Syndrome. Orthobullets. Available from: http://www.orthobullets.com/trauma/1001/leg-compartment-syndrome. Accessed 10/7/15.
Klenerman L. The evolution of the compartment syndrome since 1948 as recorded in the JBJS (B). J Bone Joint Surg Br 2007; 89:1280.
Stracciolini, A., Hammerberg, E. 2014. Up To Date. Acute Compartment Syndrome available from: http://www.uptodate.com/contents/acute-compartment-syndrome-of-the-extremities#H8 Accessed 1/7/15
 RSS Feed
RSS Feed
