Ella a 4 y.o girl RHD presented to the local ED department with R elbow pain, swelling and reduced range of movement.
True AP and Lateral Xrays of Ella’s elbow are below, please describe them and how you would approach an elbow Xray:
True AP and Lateral Xrays of Ella’s elbow are below, please describe them and how you would approach an elbow Xray:
First ensure correct film, views, and the films are technically adequate, assessment should include:
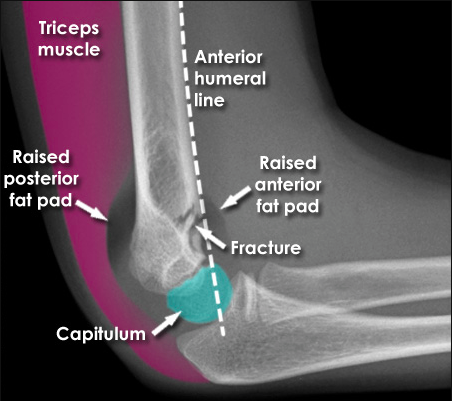
Lateral view: demonstrates an obvious fracture line on the anterior supracondylar region of the humerus, less than 1/3 of the capitellum is anterior to the anterior humeral line. There is also raised posterior and anterior fat bad and surrounding soft tissue swelling.
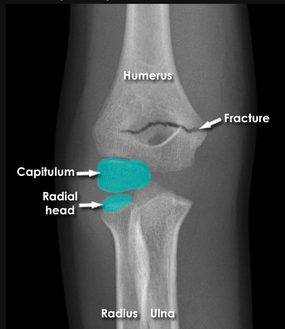
AP view: There is a visible supracondylar fracture line over the medial aspect of the humerus, no apparent intra-articular involvement, rotation, angulation or displacement in this view.
Visible fracture line
Lateral view: demonstrates an obvious fracture line on the anterior supracondylar region of the humerus, less than 1/3 of the capitellum is anterior to the anterior humeral line. There is also raised posterior and anterior fat bad and surrounding soft tissue swelling.
AP view: There is a visible supracondylar fracture line over the medial aspect of the humerus, no apparent intra-articular involvement, rotation, angulation or displacement in this view.
Visible fracture line
- Location and especially presence of articular involvement
- Angulation (use the Anterior humeral line: passes through middle 1/3 of capitellum - see image below on left. If there is a displaced supracondylar fracture this line will pass in front of capitellum, right image below )
- Alignment of the radius and ulnar with the distal humerus (use Radio-capitellar line: line drawn down neck of radius on AP film, should pass through the center of the capitellum. Assesses for radial dislocation)

Invisible fracture line: Assess for joint effusion (anterior and posterior fat pad sign)
NOTE: anterior fat pad may be normal, unless assumes ‘ship sail’ shape. Posterior fat pad may be normal if arm in extension. If uncertain immobalise and recommend re-imaging in 7-10 days)
NOTE: anterior fat pad may be normal, unless assumes ‘ship sail’ shape. Posterior fat pad may be normal if arm in extension. If uncertain immobalise and recommend re-imaging in 7-10 days)
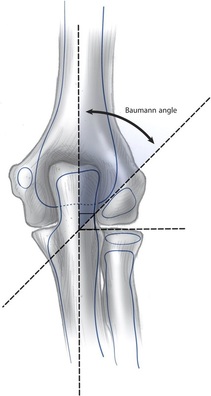
Baumann’s angle AKA humeral-capitellar angle: angle between the long axis of the humerus and the capitellar physis (line through growth plate of the capitellum) – see diagram. Normal angle 70-75 degrees (but always compare to the carrying angle of the uninjured side – a deviation of more that 5 degrees compared to other side should not be accepted)
Tear drop (AKA hour glass sign): dense line representative of the capitellum and posterior margin of coronoid fossa – indicates true lateral of elbow
You should always get an xray of the ipsilateral wrist (distal radius/ulnar fracture) and shoulder (proximal humerus fracture)
Remember to consider other elbow trauma: radial head dislocation, epicondylar fractures can mimic an undisplaced supracondylar fracture
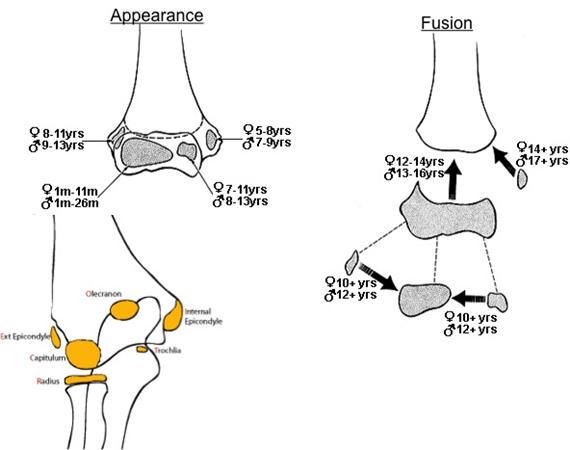
Remember ossification centres, CRITOE
Remember to consider other elbow trauma: radial head dislocation, epicondylar fractures can mimic an undisplaced supracondylar fracture
Remember ossification centres, CRITOE
What does CRITOE stand for and what is the timing of ossification centres of male and female elbow?
- Capitellum
- Radius
- Internal/Medial Epicondyle
- Trochlear
- Olecranon
- External/Lateral Epicondyle
Classify Ella’s fracture according to Gartland’s Classification (Sheth, U. Taylor, B 2015)
Ella has a Type 1 Gartland's fracture.
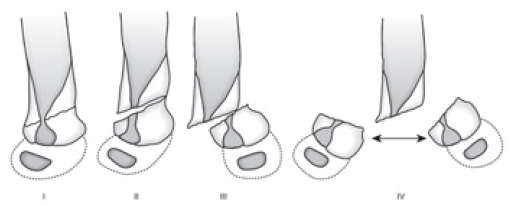
Gartland's Classification:
Type 1: Non displaced
Type 2: Displaced, posterior cortex in tact. The anterior humeral line does not intersect the capitellum. This can be further subdivided into
Type 3: Completely displaced
Type 4: (not in original Gartland’s classification): complete periosteal disruption with instability in flexion and extension
Ella has a Type 1 Gartland's fracture.
Gartland's Classification:
Type 1: Non displaced
Type 2: Displaced, posterior cortex in tact. The anterior humeral line does not intersect the capitellum. This can be further subdivided into
- 2a: minimally displaced no rotation
- 2b rotational deformity
Type 3: Completely displaced
Type 4: (not in original Gartland’s classification): complete periosteal disruption with instability in flexion and extension
Ella cannot pronate or supernate her arm, explain why she cannot do this using biomechanics of the elbow.
The elbow has two functionally independent articulations that share a synovial compartment. They are:
1. ulnotrochlear articulation directs flexion and extension
2. radiocapitellar joint governs forearm rotation
Approximately 7 % of supracondylar fractures are associated with nerve injury, what nerves would most likely be effected and how would you test these?
How would you manage Ella’s supracondylar fracture?
Always ensure patient is neurovascularly intact
Ella was managed with a closed reduction, which involved traction followed by flexion of elbow with slight anterior pressure of the posterior displaced segment and placed in a long arm posterior splint (or collar and cuff) at > 90 degrees of flexion for three to four weeks.
Repeat radiographs were taken to ensure adequate reduction and she was referred to fracture clinic in 5-7 days with repeat X-ray.
Note: Without support, the weight of the cast applies an extension torque to the distal humerus and can lead to posterior fracture displacement
How would you manage other supracondylar fractures?
Non-Operative Long arm posterior splint then long arm casting with up to 90 degrees of elbow flexion:
Operative
Immediate closed reduction and percutaneous pinning (K-wires)
Closed reduction and percutaneous pinning
Open reduction with percutaneous pinning
The elbow has two functionally independent articulations that share a synovial compartment. They are:
1. ulnotrochlear articulation directs flexion and extension
2. radiocapitellar joint governs forearm rotation
Approximately 7 % of supracondylar fractures are associated with nerve injury, what nerves would most likely be effected and how would you test these?
- Anterior interosseus nerve (branch of median nerve): Ella would be unable to make A-OK sign (cannot flex interphalangeal joint of this thumb and DIPJ of her index finger.
- Radial nerve: Ella would be unable extend her wrist or digits
How would you manage Ella’s supracondylar fracture?
Always ensure patient is neurovascularly intact
Ella was managed with a closed reduction, which involved traction followed by flexion of elbow with slight anterior pressure of the posterior displaced segment and placed in a long arm posterior splint (or collar and cuff) at > 90 degrees of flexion for three to four weeks.
Repeat radiographs were taken to ensure adequate reduction and she was referred to fracture clinic in 5-7 days with repeat X-ray.
Note: Without support, the weight of the cast applies an extension torque to the distal humerus and can lead to posterior fracture displacement
How would you manage other supracondylar fractures?
Non-Operative Long arm posterior splint then long arm casting with up to 90 degrees of elbow flexion:
- Indication: Type 1, Type 2a fractures that has no medial comminution, minimal swelling and anterior humeral line intersects the anterior half of the capitellum
- Repeat radiographs at 3-7 days and immobalisation for 3-4 weeks +/- additional time with removal posterior long arm posterior splint.
Operative
Immediate closed reduction and percutaneous pinning (K-wires)
- Indications: vascular compromise (pale, cool hand), floating elbow
- Technique: check vascular status after reduction
Closed reduction and percutaneous pinning
- Indications: Type 2b (not meeting the above criteria) and Type 3
Open reduction with percutaneous pinning
- Indication: when closed reduction was not successful, more likely if a flexion type fracture
REFERENCES
Kids Health WA. Supracondylar Fractures (2015).Available from: http://kidshealthwa.com/wp-content/uploads/2013/12/Supracondylar.jpg
Accessed: 30/8/15
Radiology Masterclass. Trauma Xrays Upper Limb. (2015). Available from: http://www.radiologymasterclass.co.uk/gallery/trauma
Accessed: 2/8/15
Sheth, U. Taylor, B. (2015) Supracondylar Fractures -Pediatric. Orthobullets. Available from: http://www.orthobullets.com/pediatrics/4007/supracondylar-fracture--pediatric Accessed: 1/8/15
Kids Health WA. Supracondylar Fractures (2015).Available from: http://kidshealthwa.com/wp-content/uploads/2013/12/Supracondylar.jpg
Accessed: 30/8/15
Radiology Masterclass. Trauma Xrays Upper Limb. (2015). Available from: http://www.radiologymasterclass.co.uk/gallery/trauma
Accessed: 2/8/15
Sheth, U. Taylor, B. (2015) Supracondylar Fractures -Pediatric. Orthobullets. Available from: http://www.orthobullets.com/pediatrics/4007/supracondylar-fracture--pediatric Accessed: 1/8/15









 RSS Feed
RSS Feed
