24 y.o male has been referred to fracture clinic query a right foot, Lisfranc injury, He presented to ED 2 days ago with inability to weightbear, forefoot pain and swelling after a tackle in a rugby game.
What is the Lisfranc ligament and why is it important?
What is the Lisfranc ligament and why is it important?
It is a ligament (depicted above in yellow) from medial cuneiform (under 1st metatarsal) to the base of the 2nd metatarsal on the plantar surface. It tightens with abduction and pronation of the forefoot.
It is integral in maintaining the midfoot arch and stabalising the 2nd metatarsal. As there is no ligament directly connecting the 1st and 2nd metatarsal.
What is the mechanism of injury usually?
Injury usually includes fall from height, motor vehicle accident or athletic injury like in this case.
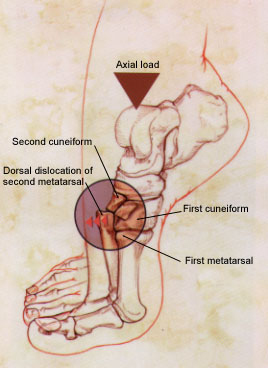
Hyperplantar flexed forefoot, compression (axial load) and abduction (indirect rotational force) transmitted to the tarso-metotarsal articulation – causing metatarsals to be displace in a dorsal/lateral direction, as depicted below.
It is integral in maintaining the midfoot arch and stabalising the 2nd metatarsal. As there is no ligament directly connecting the 1st and 2nd metatarsal.
What is the mechanism of injury usually?
Injury usually includes fall from height, motor vehicle accident or athletic injury like in this case.
Hyperplantar flexed forefoot, compression (axial load) and abduction (indirect rotational force) transmitted to the tarso-metotarsal articulation – causing metatarsals to be displace in a dorsal/lateral direction, as depicted below.
Assessing the patient:
1. Assess foot circulation
2. Assess soft tissue
3. Assess associated injury
Instability test: grasp metatarsal heads and apply dorsal force to forefoot while other hand palpates the TMT joints dorsal subluxation suggests instability
Provocative tests may reproduce pain with pronation and abduction of forefoot
What imaging would you order?
Xrays: AP, lateral, oblique 30 degrees, If possible -AP Weight bearing Xrays: comparison can be made to other side
Stress radiograph: if non-weight bearing Xrays normal but clinically high suspicion for Lisfranc stress views may be helpful to show instability
CT scan: for diagnosis and preoperative planning
MRI: diagnose pure ligamentous injury
Below are his Xrays, describe the deformity.
1. Assess foot circulation
- The anterior tibial artery has the first dorsal and first plantar metatarsal artery that supplies the medial foot, disruption of this astemosis can cause signficiant haemorrhage and compartment syndrome
- Compartment syndrome
2. Assess soft tissue
- Stellate bruising over midfoot plantar area
- Swelling, prominence of medial tarsal bones, shortening of forefoot
3. Assess associated injury
- Abduction mechanism of injury – compression fracture of cuboid, MTPJ dislocations, TMTJ fractures/dislocations, metatarsal fractures
Instability test: grasp metatarsal heads and apply dorsal force to forefoot while other hand palpates the TMT joints dorsal subluxation suggests instability
- If 1st and 2nd metatarsals can be displaced medially and laterally, global instability is present and surgery is required
- No dorsal subluxation = plantar ligaments are intact, injury may be treated non-operatively
Provocative tests may reproduce pain with pronation and abduction of forefoot
What imaging would you order?
Xrays: AP, lateral, oblique 30 degrees, If possible -AP Weight bearing Xrays: comparison can be made to other side
Stress radiograph: if non-weight bearing Xrays normal but clinically high suspicion for Lisfranc stress views may be helpful to show instability
CT scan: for diagnosis and preoperative planning
MRI: diagnose pure ligamentous injury
Below are his Xrays, describe the deformity.
What are the 5 critical radiographic signs of midfoot instability?
AP view:
1. The medial base of the 2nd metatarsal does not align with the medial side of the middle cuneiform.
2. Widening of the interval between the first and second ray
Oblique view:
3. Medial side of 4th metatarsal base does not line up with medial side of cuboid
Lateral view:
4. Dorsal displacement of metatarsal base
5. Disruption of the medial column line (line tangential to the medial aspect of the navicular and the medial cuneiform)
Flec sign (on AP view): may see bony fragment in 1st intermetatarsal space (avulsion of Lisfanc ligament from base of 2nd metatarsal)
Treatment
Non-operative: immobilization for 8 weeks Vs Operative
Indications for non-operative management?
Non-displaced on weight-bearing and stress radiographs and no evidence of bony injury on CT. OR:
What are the different operative options:
1. Open reduction and rigid internal fixation:
Indication: Any instability (> 2mm shift) and or fracture dislocations, rather than pure ligamentous injuries
2. Primary athrodesis of the 1st, 2nd and 3rd metatarsal joints
Indication: pure ligamentous injury
3. Midfoot athrodesis
Indication: unstable midfoot architecture with progressive arch collapse and forefoot abduction, chronic lisfranc injuries that have led to midfoot arthrosis and failed conservative management
Reference:
[1] Blomberg, J (2015) Lisfranc Injury (Tarsometatarsal fracture-dislocation). Orthobullets. Retrieved 20 June 2015 from http://www.orthobullets.com
[2] And Rabou, A., Gaillard, F et al. (2015) Lisfranc Injury. Radiopaeidia. Retrieved 20 June 2014 from http://radiopaedia.org/articles/lisfranc-injury
AP view:
1. The medial base of the 2nd metatarsal does not align with the medial side of the middle cuneiform.
2. Widening of the interval between the first and second ray
Oblique view:
3. Medial side of 4th metatarsal base does not line up with medial side of cuboid
Lateral view:
4. Dorsal displacement of metatarsal base
5. Disruption of the medial column line (line tangential to the medial aspect of the navicular and the medial cuneiform)
Flec sign (on AP view): may see bony fragment in 1st intermetatarsal space (avulsion of Lisfanc ligament from base of 2nd metatarsal)
Treatment
Non-operative: immobilization for 8 weeks Vs Operative
Indications for non-operative management?
Non-displaced on weight-bearing and stress radiographs and no evidence of bony injury on CT. OR:
- Non-ambulatory patients
- Severe vascular disease
- Severe peripheral neuropathy
- Instability in only the transverse plane
What are the different operative options:
1. Open reduction and rigid internal fixation:
Indication: Any instability (> 2mm shift) and or fracture dislocations, rather than pure ligamentous injuries
2. Primary athrodesis of the 1st, 2nd and 3rd metatarsal joints
Indication: pure ligamentous injury
3. Midfoot athrodesis
Indication: unstable midfoot architecture with progressive arch collapse and forefoot abduction, chronic lisfranc injuries that have led to midfoot arthrosis and failed conservative management
Reference:
[1] Blomberg, J (2015) Lisfranc Injury (Tarsometatarsal fracture-dislocation). Orthobullets. Retrieved 20 June 2015 from http://www.orthobullets.com
[2] And Rabou, A., Gaillard, F et al. (2015) Lisfranc Injury. Radiopaeidia. Retrieved 20 June 2014 from http://radiopaedia.org/articles/lisfranc-injury





 RSS Feed
RSS Feed
