Nathan 38 y.o M, police officer, presented to ED with sudden onset left heel and calf pain, immediately on jumping whilst playing basketball. He reports hearing an immediate 'pop' sound.
He was unable to weight bear due to the pain and is finding it difficult to plantar flex his foot
What are the risk factors for achilles tendon rupture?
1. Steroid injections
2. Episodic athletes
3. Fluoroquinolone antibiotics: broad spectrum antibiotics (covers gram negative and positive bacteria) often used to treat hospital acquired infections, ie pneumonia, or UTIs. Examples include: ciprofloxacin, gemifloxacin, levofloxacin moxifloxacin, and norfloxacin.
Nathan denies any of the above risk factors.
What are the main mechanisms of injury?
1. Sudden forced plantar flexion
2. Sudden dorsiflexion from foot being in a plantar position
Describe the anatomy of the achilles tendon; origin, insertion, blood supply, innervation:
The Achilles tendon is the largest tendon in the body and is a confluence of the soleus muscle tendon and the lateral and medial gastrocnemius heads. It inserts into the middle 1/3 of the posterior calcaneal surface. Supplied by the posterior tibial artery.
Achilles tendon reflex tests S1, S2
What clinical findings would you look for?
1. Obvious deformity - Obvious calf swelling/deformity. Also ask Nathan to lie in prone position and flex both knees, if there is an increase dorsiflexion of affected side this is indicative of achilles injury (as achilles tendon plantar flexes foot). There can be calf atrophy in chronic cases of achilles tendon rupture.
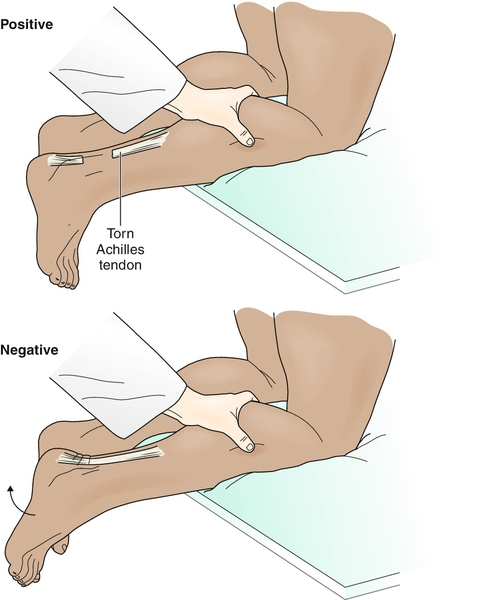
2. Squeeze test (Thompson test) - get Nathan to kneel on edge of bed/seat or move down bed so that feet unsupported and are hanging off the end. Squeeze the normal calf first and watch his foot (foot should plantar-flex then retract to neutral if achilles tendon in tact). Then squeeze calf of affected side, no movement of foot suggests complete rupture of achilles tendon - POSITIVE Thompson Test (See image below, (Stretanski, M 2015)). If there is some movement (or equivocal result), further investigations (USS or MRI) should be undertaken.
3. Step deformity: palpate along the tendon to determine whether there is an obvious rupture/disruption
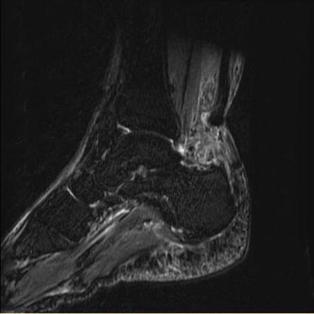
Your ED consultant conducts a quick bedside USS of the achilles tendon which demonstrates complete rupture approximately 5cm proximal from the calcaneal insertion. Why do achilles tendon's normally rupture here?
The posterior tibial artery supplies the achillies tendon, however, there is a watershed area (hypovascular region) 4-6cm from the calcaneal insertion, it is this area that is prone to rupture.
Achilles tendon injury can either be classified as complete or partial rupture.
Xrays are not diagnostic but can be useful if an associated calcaneal avulsion injury needs to be ruled out. Otherwise USS or MRI can be utilised.
What does the orthopaedic registrar need to know when you call them?
Patient information, including medical history (diabetic), occupation (athlete), smoker, risk factors
Affected side, mechanism of injury, previous achilles tendon injury
Clinical signs
Investigations: Xray, USS findings - confirmed full/partial achilles tendon rupture
Treatment Options
Conservative vs Surgical Management AGAIN!! - Historically operative management was preferred with younger, healthier patients due to a re-rupture rate of 2% compared to 11-30% for non surgical. However, a recent meta-analysis of randomised controlled trials have demonstrated there is no significant difference between re-rupture rates in operative versus conservative management, if conservative management involves aggressive functional rehabilitation protocols (Soroceanu, et al 2012). There is however, an absolute risk increase of 15.8% associated with surgery for complications other than rupture, such as infection and wound breakdown (Soroceanu, et al 2012). These results have driven a change towards conservative management with aggressive function rehabilitation rather than surgical treatment for achilles tendon ruptures.
Conservative Management:
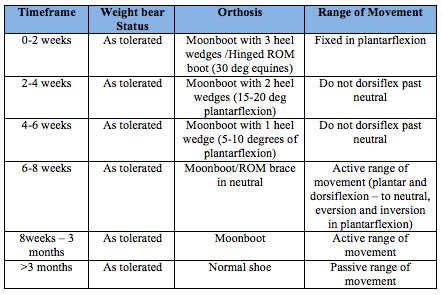
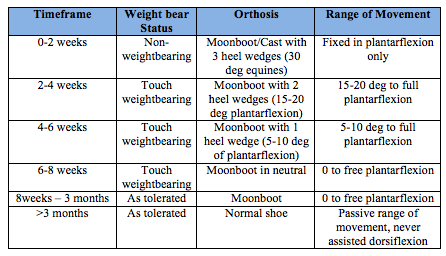
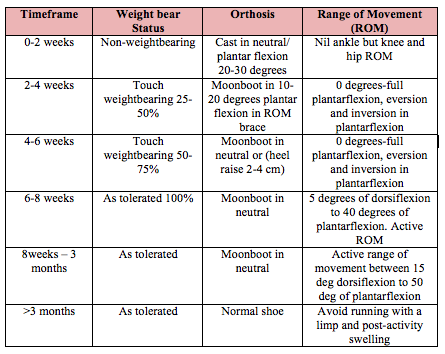
This is becoming the primary method of management for complete achilles tendon ruptures. There are many protocols available. They aim for aggressive functional rehabilitation. In the November 2015 Journal of Bone and Joint surgery, discussed a recent randomised controllled trial, Barford 35 al. which demonstrated there was no significant difference between the Achilles tendon Total Rupture Score (ATRS) and heel-rise strength in patients that weight bear day 1 post injury compared to a control non-weight-bearing (6 weeks).
Below is an example of two different conservative management protocols. The hospital or individual consultant you work for may have there own. The first is a more aggressive protocol, the second more conservative (Brunello R,et al, 2013).
Your ED consultant conducts a quick bedside USS of the achilles tendon which demonstrates complete rupture approximately 5cm proximal from the calcaneal insertion. Why do achilles tendon's normally rupture here?
The posterior tibial artery supplies the achillies tendon, however, there is a watershed area (hypovascular region) 4-6cm from the calcaneal insertion, it is this area that is prone to rupture.
Achilles tendon injury can either be classified as complete or partial rupture.
Xrays are not diagnostic but can be useful if an associated calcaneal avulsion injury needs to be ruled out. Otherwise USS or MRI can be utilised.
What does the orthopaedic registrar need to know when you call them?
Patient information, including medical history (diabetic), occupation (athlete), smoker, risk factors
Affected side, mechanism of injury, previous achilles tendon injury
Clinical signs
Investigations: Xray, USS findings - confirmed full/partial achilles tendon rupture
Treatment Options
Conservative vs Surgical Management AGAIN!! - Historically operative management was preferred with younger, healthier patients due to a re-rupture rate of 2% compared to 11-30% for non surgical. However, a recent meta-analysis of randomised controlled trials have demonstrated there is no significant difference between re-rupture rates in operative versus conservative management, if conservative management involves aggressive functional rehabilitation protocols (Soroceanu, et al 2012). There is however, an absolute risk increase of 15.8% associated with surgery for complications other than rupture, such as infection and wound breakdown (Soroceanu, et al 2012). These results have driven a change towards conservative management with aggressive function rehabilitation rather than surgical treatment for achilles tendon ruptures.
Conservative Management:
This is becoming the primary method of management for complete achilles tendon ruptures. There are many protocols available. They aim for aggressive functional rehabilitation. In the November 2015 Journal of Bone and Joint surgery, discussed a recent randomised controllled trial, Barford 35 al. which demonstrated there was no significant difference between the Achilles tendon Total Rupture Score (ATRS) and heel-rise strength in patients that weight bear day 1 post injury compared to a control non-weight-bearing (6 weeks).
Below is an example of two different conservative management protocols. The hospital or individual consultant you work for may have there own. The first is a more aggressive protocol, the second more conservative (Brunello R,et al, 2013).
Surgical Management:
1. End to end achilles tendon repair: incision is made just medial to tendon to avoid sural nerve, the paratendon is incised to expose the tendon edges and heavy non-absorable sutures are used to repair the achilles tendon.
2. Minimally invasive percutaneous tendon repair: a small transverse incision is made at the level of achilles tendon rupture, and tendon ends are identified. Sutures are passed both proximally and distally to the incision, capturing the ends of the tendon. From the incision the sutures are pulled out of the skin and paratendon so that they are only through the achilles tendon. The sutures from both ends are tied, approximating both ends of the tendon. This technique's pitfulls include limited purchase of the tendon and incidental damage of the sural nerve (0 to 10.5%) in the literature (Rouvillian 2010).
There are additional surgical techniques for chronic (> 3 months old) ruptures.
Post surgical rehabilitation protocol is then instigated. Similarly to conservative management there are multiple protocols available. Here is an example of one from the University of Wisconsin Sports Medicine and Physician group (2015):
References
Barfod KW, Bencke J, Lauridsen HB, Ban I, Ebskov L, Troelsen A. Nonoperative dynamic treatment of acute Achilles tendon rupture: the influence of early weightbearing on clinical outcome: a blinded, randomized controlled trial. J Bone Joint Surg Am. 2014 Sep 17;96(18):1497-503.
Braumann, M, Baumbach S, Mutschler W, Polzer, H. (2014) Accelerated rehabilitation following Achilles tendon repair after acute rupture – Development of an evidence-based treatment protocol. Sciencedirect. Volume 45, Issue 11, November 2014, Pages 1782–1790
Brunello R, Lutz M, Irons G, Smith C. (2013) Royal Brisbane and Women's Hospital Achilles tendon rehabilitation protocol.
Karadsheh M. (2015). Achilles Tendon Rupture. Orthobullets. Available From: http://www.orthobullets.com/foot-and-ankle/7021/achilles-tendon-rupture. Accessed 14/12/15.
University of Wisconsin Sports Medicine (2015). Available from: http://www.uwhealth.org/files/uwhealth/docs/sportsmed/SM-41576_AchillesTendonProtocol.pdf Accessed 14/12/15.
Uquillas C; Guss, M, Ryan, D, Jazrawi, L, Strauss, E (2015) Everything Achilles: Knowledge update and Current Concepts in Management. J Bone Joint Surg Am, 2015 Jul 15; 97 (14): 1187 -1195 .
Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. (2012). Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials J Bone Joint Surg Am. 2012 Dec 5;94(23):2136-43
Stretanski, M. (2015) Achilles Tendinopathy. Available from: http://clinicalgate.com/81-achilles-tendinopathy/#f0010 Accessed 14/12/15
Rouvillain JL, Navarre T, Labrada-Blanco O, Garron E, Daoud W. Percutaneous suture of acute Achilles
tendon rupture. A study of 60 cases. Acta Orthop Belg. 2010 Apr;76(2):237-42. PubMed PMID: 20503951
Barfod KW, Bencke J, Lauridsen HB, Ban I, Ebskov L, Troelsen A. Nonoperative dynamic treatment of acute Achilles tendon rupture: the influence of early weightbearing on clinical outcome: a blinded, randomized controlled trial. J Bone Joint Surg Am. 2014 Sep 17;96(18):1497-503.
Braumann, M, Baumbach S, Mutschler W, Polzer, H. (2014) Accelerated rehabilitation following Achilles tendon repair after acute rupture – Development of an evidence-based treatment protocol. Sciencedirect. Volume 45, Issue 11, November 2014, Pages 1782–1790
Brunello R, Lutz M, Irons G, Smith C. (2013) Royal Brisbane and Women's Hospital Achilles tendon rehabilitation protocol.
Karadsheh M. (2015). Achilles Tendon Rupture. Orthobullets. Available From: http://www.orthobullets.com/foot-and-ankle/7021/achilles-tendon-rupture. Accessed 14/12/15.
University of Wisconsin Sports Medicine (2015). Available from: http://www.uwhealth.org/files/uwhealth/docs/sportsmed/SM-41576_AchillesTendonProtocol.pdf Accessed 14/12/15.
Uquillas C; Guss, M, Ryan, D, Jazrawi, L, Strauss, E (2015) Everything Achilles: Knowledge update and Current Concepts in Management. J Bone Joint Surg Am, 2015 Jul 15; 97 (14): 1187 -1195 .
Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. (2012). Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials J Bone Joint Surg Am. 2012 Dec 5;94(23):2136-43
Stretanski, M. (2015) Achilles Tendinopathy. Available from: http://clinicalgate.com/81-achilles-tendinopathy/#f0010 Accessed 14/12/15
Rouvillain JL, Navarre T, Labrada-Blanco O, Garron E, Daoud W. Percutaneous suture of acute Achilles
tendon rupture. A study of 60 cases. Acta Orthop Belg. 2010 Apr;76(2):237-42. PubMed PMID: 20503951
 RSS Feed
RSS Feed
