Hamish a 28 y.o male, right hand dominant, presented to his GP with bilateral pain in his wrists and paraesthesia on the palmer aspects of his hands. The symptoms are worse in his right hand, involve all fingers except his little finger, and it wakes him from his sleep. He never has symptoms during the day. His GP suspects carpal tunnel syndrome (CTS).
What are the risk factors for Carpal Tunnel Syndrome (McKean, J 2015)?
Other aetiologies include; tumours, trauma, any cause of tenosynovitis of the flexor tendons, amyloidosis.
The GP has taken a thorough history but Hamish has no risk factors for CTS. He has never been exposed to work involved with repetitive movement or vibrations but does love playing tennis. This is the only aggravating factor identified.
What are other symptoms associated with carpal tunnel syndrome?
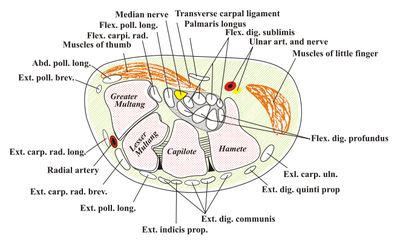
What structures are within the carpal tunnel? See below
9 flexor tendons: 4 x flexor digitorum superficialis, 4 x flexor digitorum profundus, flexor pollicis longus
median nerve.
The carpal tunnel is narrowest at level of hook of hamate.
What are the borders of the carpal tunnel? See below
The scaphoid and trapezium tubercle radially, triquetral, hook of hamate and pisiform ulnarly.
The floor is made up of carpal bones and the roof, carpal tunnel ligament.
What are the risk factors for Carpal Tunnel Syndrome (McKean, J 2015)?
- Female gender
- Obesity
- Inflammatory conditions: Rheumatoid arthritis, gout, pseudogout
- Endocrinopathies: Hypothyroidism, acromegaly, diabetes, pregnancy, OCP
- Advanced age
- Alcoholism
- Chronic renal failure
- Repetitive wrist movements
- Smoking
- Mucolipidosis
- Mucopolysaccharidosis
Other aetiologies include; tumours, trauma, any cause of tenosynovitis of the flexor tendons, amyloidosis.
The GP has taken a thorough history but Hamish has no risk factors for CTS. He has never been exposed to work involved with repetitive movement or vibrations but does love playing tennis. This is the only aggravating factor identified.
What are other symptoms associated with carpal tunnel syndrome?
- Paraesthesia, numbness often effects middle finger first, then thumb and index
- Clumsiness, dropping objects
- Pain should only radiate to the elbow
What structures are within the carpal tunnel? See below
9 flexor tendons: 4 x flexor digitorum superficialis, 4 x flexor digitorum profundus, flexor pollicis longus
median nerve.
The carpal tunnel is narrowest at level of hook of hamate.
What are the borders of the carpal tunnel? See below
The scaphoid and trapezium tubercle radially, triquetral, hook of hamate and pisiform ulnarly.
The floor is made up of carpal bones and the roof, carpal tunnel ligament.
What findings would you expect on physical examination of Hamish?
Remember to always approach physical examination systematically: inspect, palpate, neurological tests and finally specialised tests.
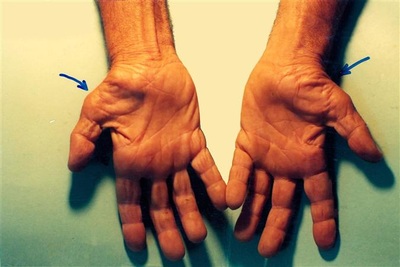
Inspect: remember to look for signs of underlying cause. For example, signs of hypothyroidism, acromegaly, previous scars, etc. Specifically:
Palpate:
Neurological Tests:
Specialised Tests:
Why does Hamish only have symptoms at night?
There are multiple factors that cause night symptoms of carpal tunnel syndrome:
The GP referred Hamish for nerve conduction studies.
What would you expect nerve conduction velocities (NCV) to demonstrate:
1. Increased latency (slowing) of NCV
Diagnosis is usually clinical and criteria include:
Management:
Once again.. always break up into non-operative and operative management.
Non-operative
1. Lifestyle changes: try to minimise the precipitating factor/aggravating factors and limit the risk factors mentioned above, ie lose weight, treat hypothyroidism, stop smoking/drinking.
2. Night splints:
To reduce nocturnal wrist flexion. This would be one of the first steps for Hamish as this is the only time he gets symptoms.
3. NSAIDS
4. Corticosteroid Injection: 80% of patients have transient improvement of symptoms, 22% remain asymptomatic at 1 year. 22 gauge needle is introduced between FCR and PL, angles 45 degrees down and distally to floor of tunnel and withdraw 5mm.
Hamish attempts the above non-operative management options but 2 years later is still experiencing symptoms. Consequently has opted for operative management.
Operative
For patient's in which conservative manaegment has failed or space occupying lesion, or acute carpal tunnel syndrome was sustained post distal radial ORIF. Temporary relief from a steroid injection is a good prognostic factor that operative management will likely give a good result for the patient.
Operative pointers:
Mark out palmaris longus tendon.
Incision is made ulnar to palmaris longus. This is in line of the fourth ray. From the level of the distal palmer crease to the level of the outstretched thumb (Do not extend past Kaplan's line - the superficial palmer arch would be found distal to Kaplan's line). Blunt dissection down flexor retinaculum, incise retinaculum from distal to proximal releasing nerve.
Pinch strength should return by 6 weeks and complete grip strength by 12 weeks.
REFERENCES
McKean, J. (2015). Carpal Tunnel Syndrome. OrthoBullets. Accessed 9/9/15. Available from http://www.orthobullets.com/hand/6018/carpal-tunnel-syndrome
Clifford R (2013). Anatomy of Carpal Tunnel. Wheeless' Textbook of Orthopaedics. Accessed 10/9/15. Available from: http://www.wheelessonline.com/ortho/anatomy_of_carpal_tunnel
Dophotoshop. (2011) Accessed 12/9/15. Available from: http://dophotoshop.com/carpal-unnel-exercises.php
Inspect: remember to look for signs of underlying cause. For example, signs of hypothyroidism, acromegaly, previous scars, etc. Specifically:
- Thenar atrophy (see image above) - late sign
Palpate:
- Compare muscle bulk from R to L
Neurological Tests:
- Thumb power: abduction, opposition and flexion (compare to contralateral side)
- Sensation: median nerve (palmer surface: thumb, index, middle and radial half of ring finger). Sensation over thenar eminence is supplied by the palmer branch of the median nerve, which enters the palm superficial to retinaculum.
Specialised Tests:
- Durkan's Test positive (carpal tunnel compression test): most sensitive test, involves using your thumbs to apply pressure on patient's carpal tunnel. Positive test if numbness or pain along median nerve distribution is elicited within 30 seconds.
- Phalen's Test: volar flexion of wrists (60 degrees). Less sensitive than Durkan's. Positive if symptoms elicited within 60 seconds
- Tinel's Test: provocation test, repetitive tapping over median nerve on volar aspect over carpal tunnel
Why does Hamish only have symptoms at night?
There are multiple factors that cause night symptoms of carpal tunnel syndrome:
- Horizontal positioning redistributes fluid (blood flow) to upper limbs. Hence why shaking arms alleviates symptoms (redistributes fluid away from carpal tunnel - decompressing nerve)
- Drainage of fluid from muscle milking/pumping is reduced
- Tendency towards wrist flexion at night
- Blood pressure drops during night, resulting in reduced perfusion pressure
The GP referred Hamish for nerve conduction studies.
What would you expect nerve conduction velocities (NCV) to demonstrate:
1. Increased latency (slowing) of NCV
- distal sensory latency of 3.2ms
- motor latencies >4.3ms
- velocity < 52m/s is abnormal
Diagnosis is usually clinical and criteria include:
- numbness and tingling in the median nerve distribution
- nocturnal numbness
- weakness and/or atrophy of the thenar musculature
- positive Tinel sign
- positive Phalen test
- loss of two point discrimination
Management:
Once again.. always break up into non-operative and operative management.
Non-operative
1. Lifestyle changes: try to minimise the precipitating factor/aggravating factors and limit the risk factors mentioned above, ie lose weight, treat hypothyroidism, stop smoking/drinking.
2. Night splints:
To reduce nocturnal wrist flexion. This would be one of the first steps for Hamish as this is the only time he gets symptoms.
3. NSAIDS
4. Corticosteroid Injection: 80% of patients have transient improvement of symptoms, 22% remain asymptomatic at 1 year. 22 gauge needle is introduced between FCR and PL, angles 45 degrees down and distally to floor of tunnel and withdraw 5mm.
Hamish attempts the above non-operative management options but 2 years later is still experiencing symptoms. Consequently has opted for operative management.
Operative
For patient's in which conservative manaegment has failed or space occupying lesion, or acute carpal tunnel syndrome was sustained post distal radial ORIF. Temporary relief from a steroid injection is a good prognostic factor that operative management will likely give a good result for the patient.
Operative pointers:
Mark out palmaris longus tendon.
Incision is made ulnar to palmaris longus. This is in line of the fourth ray. From the level of the distal palmer crease to the level of the outstretched thumb (Do not extend past Kaplan's line - the superficial palmer arch would be found distal to Kaplan's line). Blunt dissection down flexor retinaculum, incise retinaculum from distal to proximal releasing nerve.
Pinch strength should return by 6 weeks and complete grip strength by 12 weeks.
REFERENCES
McKean, J. (2015). Carpal Tunnel Syndrome. OrthoBullets. Accessed 9/9/15. Available from http://www.orthobullets.com/hand/6018/carpal-tunnel-syndrome
Clifford R (2013). Anatomy of Carpal Tunnel. Wheeless' Textbook of Orthopaedics. Accessed 10/9/15. Available from: http://www.wheelessonline.com/ortho/anatomy_of_carpal_tunnel
Dophotoshop. (2011) Accessed 12/9/15. Available from: http://dophotoshop.com/carpal-unnel-exercises.php
 RSS Feed
RSS Feed
