 [2]
[2] Steven, a 19 year old professional basketball player, presents to the ED with right shoulder pain and deformity after his arm was pulled backwards when he was defending another player in a basketball game 2 hours ago.
1. From the photo of Steven to the left, describe what you see?
There is obvious asymmetry between Steven’s shoulders, his right acromion and humeral head are prominent, his right arm is slightly abducted and internally rotated, and is being supported by his left hand.
2. Describe the likely mechanism of injury?
The shoulder is abducted and externally rotated when an anterior force is applied to the arm.
3. What focused physical examination would you undertake?
ALWAYS – check neurovascular status, rule out concurrent injuries (brachial plexus, vascular and cervicle)
5% of anterior dislocations are associated with axillary neuropraxia- should resolve within weeks. It will be difficult to assess deltoid function, therefore check dermatomal innervation (skin over distal deltoid) AND remember the entire brachial plexus is also at risk, not just the axillary nerve.
Apprehension Sign: patient is supine with shoulder off side of bed, abduct shoulder to 90 degrees and elbow to 90 degrees then externally rotate shoulder, positive test is facial expression of ‘apprehension’
Relocation Sign: decreased apprehension with anterior force applied on shoulder, when conducted apprehension maneuver descrived above.
Sulcus Sign: arm adducted by side, place inferior traction on elbow, if a depression occurs just below the acromion, then sulcus sign is positive.
4. What imaging would you order?
1. Xray – AP, lateral (scapular Y), axillary (if possible)
Other views: stryker view (shows Hill-Sacks lesion), west point view (shows glenoid bone loss)
2. CT if delayed presentation, complex fracture dislocation, osteoperotic patient
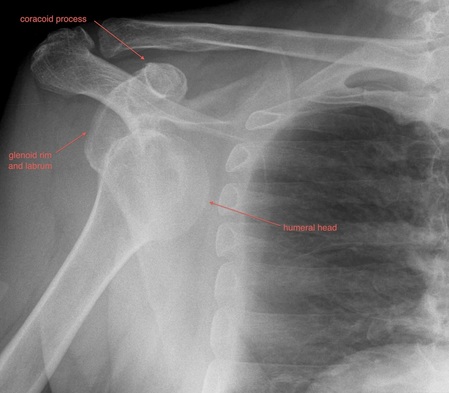
5. An AP Xray was taken of Steven's right shoulder, describe it and the diagnosis.
AP view: Head of humerus is anterior to the glenoid and inferior to the coracoid.
Always remember to ask for lateral/other views?
Diagnosis: subcoracoid anterior dislocation.
6. What closed reduction methods could you use to relocate Steven's shoulder?
Closed Reduction manoeuvres
Ensure adequate analgesia, ideally anaesthetic involvement.
1. Cunninghams Method: Ensure patient sits up straight during the entire maneuver. Have patients arm adducted, elbow at 90 degrees and arm in neutral position. Begin by firmly massaging trapezius muscle on affected side, beginning proximally and working towards shoulder, then deltoid and finally massage biceps muscle
2. Kocher’s tractionless manoeuvre: Humerus adducted, elbow flexed at 90 degrees and arm in neutral position. Then externally rotate arm and humerus (keeping humerus adducted to body) then move humerus anteriorly (keeping body still) and finally internally rotate arm.
7. You have successfully reduced Steven's shoulder, what is the next step?
1. Place in neutral brace
2. Recheck neurovascular status
3. Repeat Xrays
4. Refer to fracture clinic within 1/52
8. What injuries are associated with anterior dislocations?
1. Labral and cartilage injuries:
- Bankart Lesion: avulsion of the anterior labrum and anterior band of the IGHL – present in 80% of patients with anterior dislocations
- Humeral avulsion of the glenohumeral ligament
- Glenoid labral articular defect
- Anterior labral periosteal sleeve avulsion
2. Fractures:
- Hill-Sachs deformity: a compression fracture of the posterosuperior aspect of the humeral head
- Bony Bankart lesion: fracture of the anterior inferior glenoid
- Greater tuberosity fracture
- Lesser tuberosity fracture
References:
[1] Cunningham, N., Fennessey, G. (2012) Shoulderdislocation.net. Retrieved on 6 June 2015 from http://shoulderdislocation.net/anatomy/dislocated-anatomy
[2] Matthew, S., Stevenson, H. Physio-pedia. Retrieved on 6 June 2014 from http://www.physio-pedia.com/Shoulder_Dislocation#References







 RSS Feed
RSS Feed
